Service case study: Addressing COVID-19 vaccine hesitancy in targeted communities of Tower Hamlets.
Addressing COVID-19 vaccine hesitancy was a programme provided by community pharmacies in Tower Hamlets, East London. Utilising existing community pharmacies and their knowledge base, the aim of the service was to provide targeted interventions with underserved population groups to address the main barriers of access to COVID-19 vaccination and subsequently improve the vaccination uptake.
The service was commissioned to run from June 2022 to December 2022.
Background
The Office of National Statistics data for 2021 showed that 44.4% of Tower Hamlets residents identified their ethnic group as Asian, Asian British or Asian Welsh, 7.3% identified their ethnic group as Black, Black British, Black Welsh, Caribbean or African and 5% of people identified their ethnic group as Mixed or Multiple. Estimates suggest that 75% of Black, Asian, and minority ethnic (BAME) people were concerned about accessing the vaccination programme and some people were concerned about the content of the vaccine.
While there were no firm vaccine hesitancy figures and hesitancy rates for the area, the general picture in Tower Hamlets was that significant numbers of residents remained unvaccinated. Left unchecked, it could have led to an increase in COVID-19 cases and outbreaks, hospital admissions, and mortality rates.
Rates of vaccinations in Tower Hamlets (as of 1st of May 2022) indicated:
1st Dose: 68% (London rate 69.7%)
2nd Dose: 61.7% (London rate 64.9%)
Booster Dose: 40.1% (46.5%)
Harnessing the strength of community pharmacy
In commissioning the service, the benefits of using community pharmacy were considered:
- Community pharmacists have wider functions and influence that provide leverage when local populations access their services/collect medication. They support people to be informed about their medication (including COVID-19 vaccinations).
- Pharmacists are trusted healthcare professionals who often come from a similar cultural or ethnic background to their patients and have an opportunity to dispel myths and improve health literacy about COVID-19 vaccinations. This helps ensure standardisation of information about COVID-19 vaccination to support informed decision making.
- Familiarity and relationship building – local population are already connected to their pharmacists and therefore, more likely to trust the information.
Scope of the service
Pharmacists had one to one conversations with targeted population groups, i.e., those who were more likely to be vaccine hesitant, when they visited the pharmacy. Pharmacists were also able to provide remote consultations via telephone and video calls, for those who were more digitally advanced.
Where commissioned to provide COVID-19 vaccinations, pharmacists could then offer to provide the vaccinations in house. Ensuring these conversations were patient centered and the patient would not feel pressurised to have a vaccination, patients were offered the option to leave the pharmacy and take time to reflect on the discussion and to return subsequently if they choose to be vaccinated.
Pharmacies also worked with nearby care homes to improve vaccination rates among care homes staff.
Pharmacies were remunerated per consultation once the minimum dataset was reported via a PharmOutcomes template.
Outcomes and potential impact
In total, 3,098 consultations were carried out over the commissioned period with conversations spanning all age ranges.
Age range profile
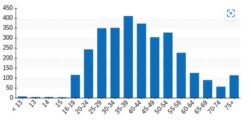
1,401 (45.2%) patients decided to get vaccinated post consultations, 865 (27.9%) were still undecided and 832 (26.9%) declined to get vaccinated.
Of the patients who decided to get vaccinated post consultation, 774 (55.2%) were offered a vaccination in house. 33 (2.4%) patients were referred to their GP, 155 (11.1%) were referred to a local vaccine centre and 439 (31.3%) decided to book their own appointments.
The data highlights the potential community pharmacy has to increase vaccine uptake in vaccine hesitant populations by having more informative conversations with patients. It also indicates the crucial role and impact that pharmacies have within the community at improving access, with 55.2% of patients choosing to get vaccinated in pharmacy.
Speaking about the service, Shilpa Shah, Chief Officer of Community Pharmacy North East London, said:
“This service demonstrates the importance of the word community in community pharmacy.
“This service was successful because people working in community pharmacies are from the same communities as their patients and the patients trust them.
“Accessibility into community pharmacy is also key, as people do not need to have an appointment and can walk in at any time. The service was opportunistic and demonstrates how innovate you have to be to reduce health inequalities and how community pharmacy can really help with this.
“Going forward, I would like to see more innovative local services being funded by Public Health teams, as the return on investment for a service like this is so beneficial for the patient and the NHS”.
More information on the vaccine hesitancy service can be found under Intervention Services on the Community Pharmacy England Services Database.







