Shared Care Records (ShCR)
Published on: 18th July 2019 | Updated on: 17th October 2023
 Shared Care Records (otherwise known as ‘ShCR’, ‘Local health and shared care records’, ‘LHCRs’ or simply ‘records’) are patients’ electronic health records. ShCRs include information from various care settings e.g. GP practice and secondary care. The majority of English patients live within an area with a records project ongoing.
Shared Care Records (otherwise known as ‘ShCR’, ‘Local health and shared care records’, ‘LHCRs’ or simply ‘records’) are patients’ electronic health records. ShCRs include information from various care settings e.g. GP practice and secondary care. The majority of English patients live within an area with a records project ongoing.
Shared care records are emerging across the country and the IT has been maturing so that over time more health and care professionals can access these and more easily. In some areas LPCs have identified their ShCR project team from the records list and worked with the ShCR project team so that pharmacy teams can access ShCRs.
Community Pharmacy England is supportive of Local Pharmaceutical Committees (LPCs) and local pharmacy contractors supporting community pharmacy involvement and ability to access and record into these records so that pharmacy team members can access or record information at the right time to better support patient care. ShCRs provide a back-up for Summary Care Records (SCRs) but also include richer information compared to SCR. The NHS Long Term Plan set out that ShCRs should eventually replace the need for frequent use of the SCR.
NHS England previously announced areas chosen to become ‘Local health and shared care record exemplar’ (LCHREs) project areas. LHCREs are a group of organisations working in collaboration to create a safe, secure and trusted information-sharing environment. These partnerships received funding to put in place an electronic shared local health and care record which makes relevant patient records available more quickly to those involved in that patient’s care and support.
ShCRs contain extra information compared with SCR with Additional Information – e.g. important vaccine information.
ShCR project teams plan to get more information into records beyond the limited GP record and to include more hospitals information, community health teams and social care, specialist clinics etc. to enable those caring for patients to have a fuller picture – reducing the need for patients to repeat themselves and protecting them from higher risks when medicines information is ‘missing’ to the community pharmacy.
Community Pharmacy England and the Community Pharmacy IT Group collated feedback explaining the critical need:
Community pharmacy contractors in Dorset are connecting to health and social care records held within the Dorset Care Record (DCR), a type of ShCR system.
Background
Primary care professionals, including community pharmacists, have been creating electronic records of their interactions with patients for many years. Previous consideration was given to the NHS creating a national comprehensive records system, collating information from different types of care settings, but the NHS Long Term Plan changed the focus to continuing and expanding the records projects being undertaken across England.
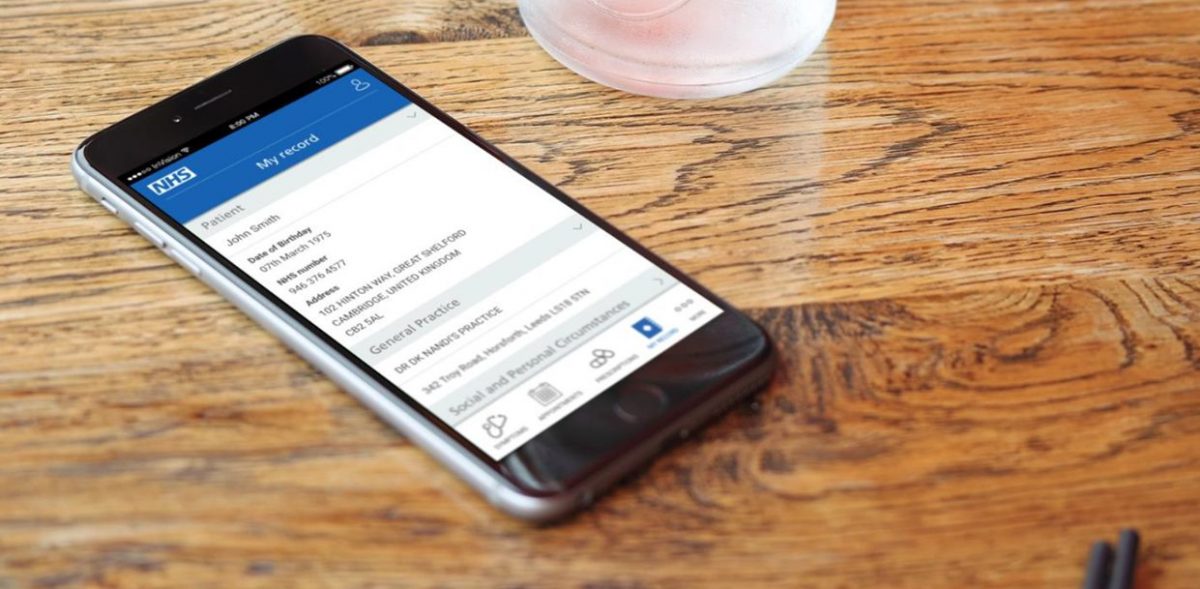
ShCRs pull together information on a patient from several sources, such as GP and hospital records, so they contain extra information compared to the NHS Summary Care Record. In time it is hoped that pharmacy systems may be able to display medicines information from ShCRs and more professionals across multiple care settings will be able to share their patient records held in their clinical systems via records.
Community Pharmacy England and the Community Pharmacy IT Group (CP ITG) encourage contractors and LPCs to get involved with records projects within their area.
What is the Dorset Care Record (DCR)?
The DCR collates records from hospitals, GPs, local authorities and Dorset HealthCare, so it contains extra information when compared with the NHS Summary Care Record Additional Information (SCR AI). Community pharmacists have been given access to the DCR to give them a fuller picture of the patient’s medical and care history. The record reduces the need for patients to repeat themselves and lessens the risks of medicines information not being visible to the pharmacists and technicians.
Benefits
Community pharmacy professionals can use DCR to:
- get an idea about medicines adherence before speaking to patients, which helps optimise consultations and the provision of services;
- care for those patients after discharge from hospital;
- check blood results to assist with medicines discussions;
- support professional decisions regarding emergency supply options;
- see why a particular medication was started (sometimes missing from SCR AI); and
- carry out an additional check if medicines have changed or stopped, to help make sure that the right medicines are available for the patient.
Community pharmacy is the first sector outside the acute and community hospital and social care settings to be given access to the DCR portal, and Dorset Local Pharmaceutical Committee (LPC) has been actively supporting the project.
How one North Dorset pharmacist used DCR?
David Rose, who runs the independent Marnhull Pharmacy in North Dorset, says his pharmacy, which is next door to the village surgery, has been massively busy.
“We’ve found that patients have come to us rather than to the GP surgery to help them with their prescriptions. Sometimes, they’ve found that the computer has said “no” and we’ve had patients who don’t understand why. We can look at the DCR to get an idea about their medicines before speaking to patients, which helps improve consultations.”
Some examples of how the pharmacy has used the DCR recently to resolve issues include:
- Looking at letter from Dorset County Hospital which are visible on the DCR. A patient was asking if eye drops had been prescribed after an ophthalmology appointment. The patient had phoned the GP surgery but had not waited as had been told he was twelfth in the queue. The letter said no treatment needed now but will be reviewed a follow up appointment.
- Helping a patient deal with a GP prescription for two strengths of Co-Beneldopa which did not make sense. The DCR showed the GP had forgotten to cancel the lower strength prescription.
- Aiding a patient who had not received an expected prescription despite having telephone consultations with their GP. The DCR GP record section showed the prescriber sometimes forgot to issue.
- Telling a patient that they could not issue Methotrexate for rheumatoid arthritis – the pharmacist could see on the DCR that a blood test was overdue.
His team is using the DCR regularly and he believes it contains extra information not available in other systems that they use and helping ensure patient safety: “We are using the DCR to ensure we prevent errors before they occur.”
And he has also been encouraging other pharmacists to use the DCR more often – saying the up to date information, particularly around discharge medications is extremely useful.
Other reflections on community pharmacy access to the DCR
Robin Mitchell, from Victoria Park Pharmacy in Dorchester has been using the DCR and reflected that:
“Access to the DCR provides community pharmacists with detailed information that complements other sources such as SCR and will be very relevant to situations such as hospital discharge or minor illness consultations. A welcome resource.”
Amanda Moores, Chief Officer at Dorset LPC added:
“We are very pleased that community pharmacies will have access to the DCR. This supports their integration in the local health and social care system. Community pharmacies play a key role in supporting patients to make the most of their medicines and manage long term conditions. The DCR supports patient care by providing pharmacies with access to up to date information, which is crucial, especially in these challenging times.”
And Peter Gill, DCR Senior Responsible Officer said:
“We are also introducing discharge medications into the Dorset Care Record from Dorset County Hospital and this will be particularly beneficial for community pharmacies.”
Advice for contractors within Dorset
Community pharmacies across Dorset have been contacted about how to connect to DCR and obtain login details. Contractors within the area can find out more at Dorset LPC’s DCR webpage, the DCR website or by contacting the DCR project team.
Further info
Read more about records projects and how to get involved at: On this webpage; Electronic health records; and Community Pharmacy England’s list of local and national record projects.
The announced areas:
| Local health and shared care record exemplar areas may include: | Local Pharmaceutical Committees (LPCs) areas may include: | Community Pharmacy LHCRE champion(s) include: |
| Yorkshire and the Humber (covering West Yorkshire, South Yorkshire, North Yorkshire and Humberside) | Community Pharmacy Humber; Community Pharmacy West Yorkshire; and Community Pharmacy North Yorkshire | David Broome |
| Thames Valley and Surrey (covering Buckinghamshire, Oxfordshire, Berkshire and Surrey, Wessex) | Bucks LPC; Pharmacy Thames Valley; and Community Pharmacy Surrey & Sussex | James Wood |
| Greater Manchester | Greater Manchester LPC | (Being selected) |
| Wessex | Dorset LPC, Community Pharmacy South Central | Amanda Moore (Chief Officer, Sefton LPC) and Deborah Crockford (Chief Officer, Community Pharmacy South Central) |
| One London |
South London: Bexley, Bromley & Greenwich LPC; Croydon LPC; Kingston, Richmond & Twickenham LPC; Lambeth, Southwark & Lewisham LPC; and Sutton, Merton & Wandsworth LPC.
North London: Barnet Enfield and Haringey; Brent and Harrow LPC; Camden & Islington LPC; City & Hackney LPC; Ealing, Hammersmith and Hounslow LPC; Hillingdon LPC; Kensington, Westminster & Chelsea LPC; Middlesex Group of LPC; and North-East London LPC |
Vikesh Patel |
Contacting pharmacy records champions: ShCR project teams that would like to get in contact with the pharmacy records champion for their area can contact it@cpe.org.uk so that Community Pharmacy England can connect the records project team to the pharmacy records champion(s).
Digital Health News reported further areas expected to be funded may include: Lancashire and South Cumbria plus Cheshire and Merseyside, the Great North Care Record and the South West. Those areas might be subject to change.
Media updates: Dorset Care Record blog update.
Even non-exemplar areas will have local records project (see the ‘List of records projects’).
Engagement and next steps
Community Pharmacy England encourages organisations that are working on local record sharing initiatives to contact local community pharmacy contractors and Local Pharmaceutical Committees (LPCs) to discuss how they may be able to participate in local developments. Community Pharmacy England has also prepared a Community Pharmacy England Briefing: Principles for implementing pharmacy access to local records.
Pharmacy contractors or LPC representatives that attend records-related events may wish to familiarise themselves with the briefing above.
LPC chief officers and members, as well as pharmacy contractors supporting pharmacy access to records information may also request to join the Community Pharmacy Digital records sub-group. Please contact Community Pharmacy England’s IT team with ‘Records group’ in the title to ask to join.
Technical challenges
If the records information is stored within the ‘nww’ area of the internet given that community pharmacies do not yet have access blanket access then the supplier’s aggregator may need to whitelist the relevant nww addresses. A list of pharmacy aggregators is found at: HSCN/N3/aggregators. If your system supplier is managing your HSCN/N3 connection they can contact the aggregator to ask that relevant nww addresses are fully whitelisted. Your pharmacy system supplier might also need to whitelist addresses as well. For a template form contact it@cpe.org.uk to assist with this process. The ShCR managers may need to provide a complete and stable list of nww addresses for the aggregators to use.
ShCR recent and future events
- ShCR meeting for CP ITG and LPCs 2021 previously occurred: Agenda and update Shared Care Records (ShCR) papers; and the Outputs and next steps and survey results document and summary of actions were published
- Bedfordshire, Luton and Milton Keynes (BLMK) ShCR event, Wednesday 2nd November 7:30pm
- Connecting with & benefitting from patient records webinar (8th December 2022 9.30am-11am, virtual event)
- ShCR summit – hosted by York and Humber ShCR project team (20th-21st March 2022, in-person event)
(No other upcoming events have been reported to Community Pharmacy England as occurring soon/recently.)
Please contact Community Pharmacy England’s IT team if there is an upcoming records event that is open to volunteers, and which can be listed here.
Actions and guidance for LPCs, contractors and others supporting the ShCR agenda
A group of LPC representatives and CP ITG agreed during a summer 2021 meeting that LPCs which had not yet done so should identify and confirm to Community Pharmacy England their local ShCR projects.
ShCR next steps for LPCs are:
- Identify the ShCR project team from the List of records systems;
- Confirm the ShCR internally within the LPC and onto the CP ITG / LPCs ShCR spreadsheet (which Community Pharmacy England circulated to LPCs);
- Learn about case studies such as: Dorset Care Record ShCR pharmacy access case study; East London Patient Record (eLPR) pharmacy case studyand the recently published Somerset Shared Care Record case study (SIDeR);
- Review the ShCR request letter (see Community Pharmacy England/RPS ShCRs/SCR letter to NHS orgs about records access);
- Contact the ShCR project team and local partners to find out how to get involved and relevant ShCR contact points (a template letter can be obtained by contacting it@cpe.org.uk);
- Use guidance to inform engagement i.e. the ‘Planning pharmacy access briefing’ and this webpage;
- Request technical info for pharmacy whitelisting: ask the local ShCR project to have its technical lead forward information to the LPC and it@cpe.org.uk (ShCR web address(es); ip address; and ip port number) so that suppliers, aggregators can be asked to whitelist at their end within the next round of whitelisting.
- Attend any local or national ShCR event opporunities.
If you have questions about these steps you may request clarification by contacting it@cpe.org.uk.
The Professional Record Standards Body (PRSB) is working with NHS England to support LHCREs. This work aims to standardise the core information that’s shared in a local health and care record so that the information that’s needed by health and care professionals can be available at the right time to better support patient care. PRSB’s view is that it is also important that information can be easily accessed even if a patient is in a different part of the country.
PRSB explain their intention with the development of their standard for a local records core dataset.
Frequently asked questions on the topic have been answered on their PRSB ShCR FAQ webpage.
IG framework for ShCRs
NHS Transformation Directorate with the support of a ShCR IG steering group has developed a ShCR IG framework (first published September 2021). The framework is intended to help Integrated Care Systems (ICSs), ShCR project teams, LPCs and others demonstrate compliance with the law, gain trust from patients and provide consistency of approach and reduce burden for patients and healthcare professionals. Community Pharmacy England has pressed for the framework to be compatible with the principle that information that’s needed by health and care professionals can be available at the right time to better support patient care.
LPCs, where required, can contact Community Pharmacy England’s IT team if they become aware of ShCR managers that state to LPCs in writing that IG reasoning is delaying pharmacy access to ShCR information. Community Pharmacy England can use such email examples during its discussions with the NHS Transformation Directorate ShCR and data policy teams.
Data sharing agreements
The NHS Transformation Directorate ShCR framework advises that data sharing agreements can support all those involved with populating or using a local Shared Care Record systems.
Signatories might include: the ShCR project team, the integrated care board (ICB), health and care organisations (individually or collectively).
An LPC may consider approving of a data sharing agreement on behalf of the contractors within its area depending on the content, although use of ShCR would be voluntary for each contractor, and it may be that the ShCR would need for each pharmacy to individually sign the agreement.
Information Commissioner’s Office (ICO) advice on data sharing agreements is that these should use “clear, concise language that is easy to understand”, although feedback to Community Pharmacy England is that this is not yet always the case within all ShCR areas.
The NHS Transformation Directorate ShCR framework references an NHS template data sharing agreement which might be used for ShCR or other purposes.
Top tips for LPCs involved with creation of data sharing agreements:
- Use clear, concise language that is easy to understand.
- Avoid duplicating reference to existing legal duties.
- Ensure the document is user tested with health and care staff.
- Be aware that pharmacy teams will be extremely busy and therefore the document should not be longer than it needs to be. Seek to keep documents short and accessible
- Recognise the document may have been prepared for various sectors including sectors which do not yet complete the Data and Security Protection Toolkit
Beginning to access local records
Community Pharmacy England’s recommendations are that:
- contractors within areas in which pharmacy contractors have ability to access the ShCR system, urgently take up this important opportunity; and
- contractors and LPCs continue to support pharmacy access.
Community Pharmacy England and RPS wrote to NHS England and NHS Improvement (NHSE&I), NHS Digital and NHS Transformation Directorate to explain that all pharmacists need be able to access ShCR systems wherever they are put in place and whichever pharmacy clinical system is being used. Read the letter in full here.
Liability
The General Pharmaceutical Council comments regarding liability:
“Pharmacists’ access to patient medical records is a welcome and positive step towards enabling pharmacy professionals to deliver improved outcomes for patients. We believe that access to records will increase dialogue and communication and improve collaboration with other healthcare professionals. Whilst this is not a new area for some of the profession, for example those working in hospitals or those who work as prescribers, we recognise that this is a developing area for community pharmacy.
A pharmacy professional’s responsibility is to make the care of patients their first concern. Pharmacy professionals who can access patient medical records must ensure that they apply the principles and requirements of conduct, ethics and performance to any additional information that they can access as result of these changes. Our standards make clear a Pharmacy professional’s responsibility in relation to confidentiality and consent, as well as ‘getting all the information you require to assess a person’s needs in order to give the appropriate treatment and care.
Pharmacy owners are required to meet the GPhC’s Standards for Registered Pharmacies. Under the first principle in those standards, concerning governance, standard 1.7 requires information to be managed so as to protect the privacy, dignity and confidentiality of patients and the public who receive pharmacy services. Our inspectors would explore the pharmacy team’s use of the record as one evidence source when assessing the pharmacy’s performance against the standard.”
National Pharmacy Association (NPA) comments regarding liability:
“NPA indemnity Insurance will cover members’ access to the Shared Care Records (ShCRs) and the Summary Care Record (SCR) (and associated liabilities in accordance with members’ PI/PL policies) where the pharmacist/pharmacy technician considers it necessary to do so (as well as any amendments the pharmacist/pharmacy technician decides to make to the ShCRs/SCRs when this facility is enabled and available in the future) provided that this is done in line with available published guidelines, the pharmacy’s standard operating procedure (SOP) governing consent and access to ShCRs/SCRs and use of the information therein.”
Local records and SCR access
Contractors with access to ShCRs may opt to access a patient’s ShCR record as an alternative to accessing a patient’s SCR record, for relevant scenarios, given that ShCRs contain more and richer information. However, even contractors with a ShCR system available to them, and that use ShCRs often, SCR is a useful back-up (in case the records system experiences an outage).
An ability to be able to access to SCR is also part of the pharmacy terms of service.
ShCRs provides additional information in comparison to Summary Care Record (SCR).
Pharmacy teams report that there are scenarios for them in which viewing ShCRs is a good alternative instead of having to access the SCR or contact the GP practices.
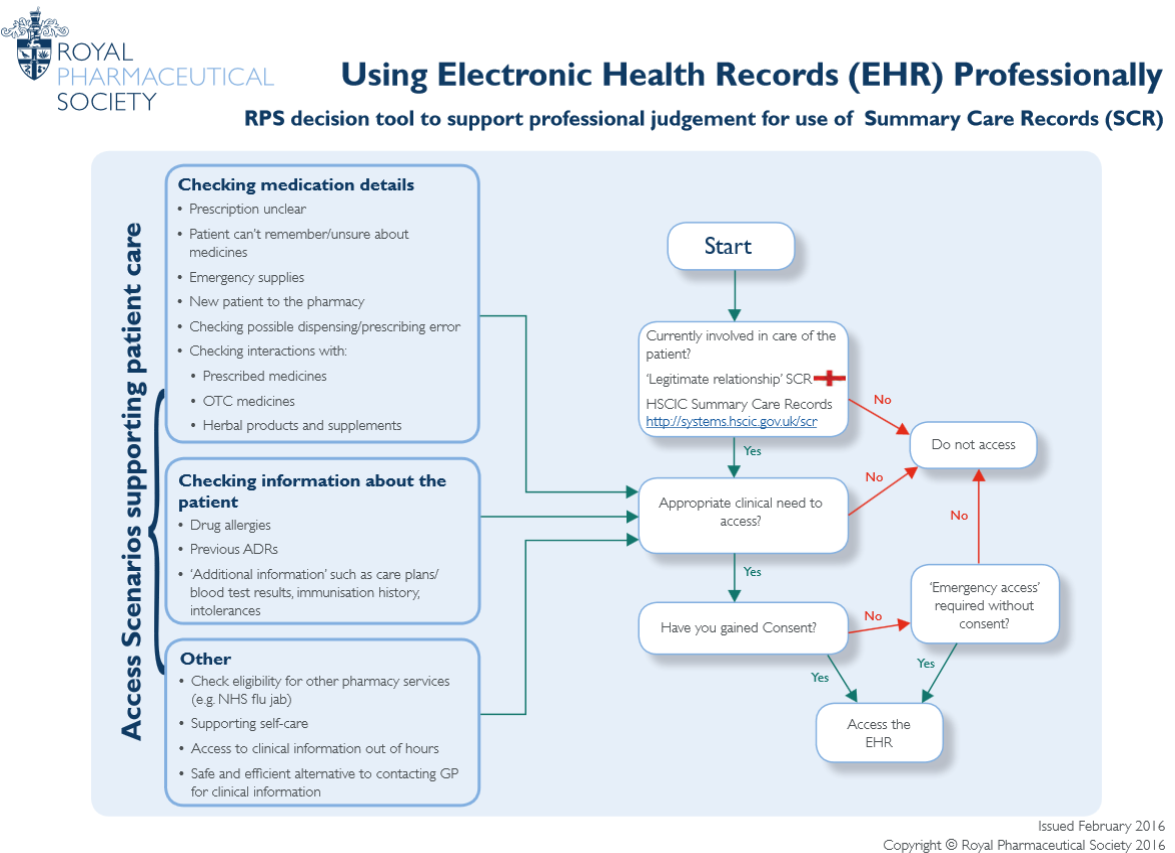
The Royal Pharmaceutical Society (RPS) has published a one-page factsheet which explains the scenarios in which to use the health records. The decision as to when to use health records is a professional one.
Listed scenarios
Checking medication details
• Prescription unclear
• Patient can’t remember/unsure about medicines
• Emergency supplies
• New patient to the pharmacy
• Checking possible dispensing/prescribing error
• Checking interactions with:
• Prescribed medicines
• OTC medicines
• Herbal products and supplements
Checking information about the patient
• Drug allergies
• Previous ADRs
• ‘Additional information’ such as care plans/blood test results, immunisation history, intolerances
Other:
Check eligibility for other pharmacy services (e.g. NHS flu jab)
• Supporting self-care
• Access to clinical information out of hours
• Safe and efficient alternative to contacting GP for clinical information
In the future, pharmacy system suppliers as well as other clinical system suppliers will be able to display information from ShCRs. Initially, it is expected many local ShCRs programmes will need to make use of online portal systems for some health care settings including the community pharmacy sector, but the logical direction of travel should be for clinical system supplier integration.
PRSB set out: Use of the Core Information Standard in community settings including pharmacy. PRSB engagement work identified the CIS is fit for use in community pharmacies, and will “complement the introduction and expansion of local ICS shared care record developments.
CP ITG discussed several related items when it prepared its 2022 Digital transformation in the NHS consultation response:
- GP Connect records IT standards should be aligned to those IT standards used by Shared Care Record (ShCR) systems.
- The Professional Record Standards Body should be commissioned to further outline the Core info standard relating to the ShCR standard and a community pharmacy subset and to enable GP Connect and ShCRs to align under the same IT standards framework. The CP ITG welcomes the work by PRSB to develop the Core Information Standard, which aims to create a standard that others could use when setting out electronic health record structures.
- The Professional Record Standards Body should with partners, including the NHS Transformation Directorate interoperability team and NHS Digital, seek to code the ShCR standards so that suppliers can more easily align and integrate into ShCRs.
- Shared Care Records (ShCRs) systems should follow aligned IT standards that should be mandated to follow the expected PRSB and coded standards.
- Shared Care Records (ShCRs) systems should follow aligned processes and health, and care workers should follow the same IG processes, training and sign-up procedures regardless of the geographic setting of the Shared Care Record (ShCR).
Integration standards: Community Pharmacy IT Group (CP ITG) have identified that there needs to be a standard approach for supplier integration with any ShCR system so that the same supplier can easily integrate with many of the ShCR systems if integrated with a single one of them. This feedback was passed to NHS Digital to help inform its standards work.
Q. What clinical information is within patients’ ShCRs? Why would I use them?
ShCR records may include more than SCR with Additional Information records i.e. the ShCR ‘fields’ may include:
medicines, allergies, notes, adverse reactions, reason for medication, immunisations, significant diagnoses / problems, significant procedures, end of life care information and patient preferences, other anticipatory care preferences, and more.
The Professional Record Standards Body (PRSB) worked with health and care staff to develop an expected template for that information which can be accessible within ShCRs. That ‘ShCR standard’ may be further developed as ShCRs becomes more widely used. In the years ahead health and care staff may access systems that enable the right information to more easily be recorded into the right place of the ShCR (e.g. greater use of ‘structured’ relevant fields and lesser use of ‘free-type’ notes fields.
Q. Would accessing a patient’s ShCR provide an alternative to accessing their SCR?
If you have access to ShCRs within your area, then use of the ShCRmay provide an alternative to use of SCR for some situations.
There is a requirement in the terms of service for NHS pharmacists who use SCR to use it, if they consider, in their clinical judgment, that it is in the best interests of the patient to do so. However, many contractors will opt to use ShCRas an alternative and may therefore determine they will not need to also access the SCR, depending on the scenario.
From 9th November 2020, pharmacy contractors have also had to ensure that relevant staff working at their pharmacy can access SCR and that access is consistent and reliable during the pharmacy’s opening hours, in so far as that is within the control of the contractor. This requirement remains in place given that:
- SCR provides a contingency option to a pharmacy contractor with access to a ShCR system (in case the ShCR system goes down);
- many pharmacy contractors do not yet have access to ShCRs; and
- there might be scenarios where a contractor with knowledge of their ShCR system and knowledge of SCR and its interface, opts to use SCR.
Pharmacy contractors have also reported to Community Pharmacy England that in future they would like for clinical systems to be able to integrate with SCR/ShCRs so that separate portal access would not be needed.
Q. My service specification or SOP states that I need to check SCR, but I have access to the ShCR and my ShCR has the same info and more. Can I use ShCR instead of SCR?
Yes. Many specifications and SOPs will reference SCR given that ShCRs are a new development and given that many areas do not yet enable ShCR access by the community pharmacy professionals.
Over time, specifications and SOPs are anticipated to be updated to specify that a relevant record (e.g. SCR/ShCR) will be able to be used. See also: the FAQ immediately above.
Q. If Shared Care Records are available for my locality am I required to use ShCR? Am I required to use ShCR for Discharge Medicines Service (DMS)?
No. There is no requirements in the regulations to access ShCRs. The ShCRs are not easily available for all pharmacies. And ShCR information is not yet integrated into clinical systems. Community Pharmacy England supports greater ShCR standardisation of IT and governance, so that in future more pharmacies have ShCR have access, and have easier access (i.e. ShCRs are integrated into existing clinical systems). As an interim ‘stepping stone’, some pharmacy teams will be granted access to ShCR portals, and determine when to access ShCR as appropropriate. However, NHS England documentation regarding DMS sets out the minimum dataset which must be transferred directly to the pharmacy team, so the trust notifying the pharmacy and asking them to check a ShCR portal does not meet that requirement.
If required Local Pharmaceutical Committees – even those many LPCs which support ShCR pharmacy access, may explain to the locality that ShCRs access is not a requirement of the DMS process.
Community Pharmacy England recognises any local ability to access ShCRs as a positive step forward for pharmacy teams, their patients and their locality. However, this does not detract from the fact tusts must send DMS referral notifications which are compliant with the minimum dataset set out. Within areas in which ShCR is available, pharmacy owners must weigh up whether to access ShCR systems, and ShCR systems access may increase as NHS England supports Integrated Care Boards (ICBs) with more standardisation.
Some pharmacy organisations may not yet have the technical ability to access ShCR systems, given that each ShCR system currently has separate technical arrangements. It is hoped that NHS ENgland’s Transformation Directorate will better support ICBs and ShCR teams with a more standardised model in the future.
Q. Are there standard data security and information governance (IG) arrangements which support the appropriate use of ShCRs?
NHS Transformation Directorate developed a ShCR IG Framework. It intends to support appropriate operational and technical arrangements but enable health and care staff have the necessary access to information for providing patient care.
Q. Will PMR suppliers and other clinical suppliers be able to read ShCR information and enable health and care staff to also record into ShCRs?
Initially it is expected ShCRs will mainly be used in many sectors via online portal systems. In the longer term, pharmacy system suppliers as well as other systems used by other clinicians may be able to display information from ShCRs as well as enable health and care staff to record relevant auditable data into the records. PMR suppliers may increasingly enable integration with SCR and ShCR information in the future.
PMR suppliers have reported to the Community Pharmacy IT Group (CP ITG) that they would like for NHS Transformation Directorate and NHS Digital to further explore whether a standard process should be developed for integrating with any ShCR project. This would enable clinical system providers to more easily integrate with multiple ShCR projects.
Further info
Read more at:
- Principles for setting pharmacy access to local records (briefing)
- LHCREs (NHS England and NHS Improvement)
If you have queries on this webpage or you require more information please contact it@cpe.org.uk. LPC chief officers and members, as well as pharmacy contractors supporting pharmacy access to ShCR information may also request to join the Community Pharmacy Digital Local health and care records (LHCRs) sub-group. Please contact Community Pharmacy England’s IT team with ‘ShCR group’ in the title to ask to join.