Community Pharmacy IT Group (CP ITG) workstream updates
Published on: 28th June 2021 | Updated on: 11th September 2025
Read more about CP ITG and its work at: the Community Pharmacy IT Group (CP ITG) webpage.
This ‘CP ITG workstream update‘ webpage sets out information following CP ITG meetings based on the the latest pharmacy IT bulletin.
The latest bulletin can also be downloaded in pdf format: CP ITG Autumn 2025 IT bulletin (pdf)
CP ITG has five workstream areas:
- Interoperability and security: Ensuring information about people’s health and care can be safely and securely accessed, wherever it is needed. (WS1a-1d)
- Reducing burden: Use of digital to reduce the burden on pharmacy teams, so they can focus on patients, and appropriate infrastructure for the task. (WS2a)
- Good use of digital: Support the use of digital within pharmacy to improve health and care productivity, improve patient safety outcomes and improve cooperation between pharmacy teams and the health and care system. (WS3a-3c)
- Patient and pharmacy tools: Support enabling patients to be able to choose digital tools to access medicines information and pharmacy services directly, so they can receive the best outcomes, recognising the need to also remain inclusive for all patients. (WS4a)
- Set out roadmap priorities: Development and promotion of a wider community pharmacy digital roadmap / vision. (WS5a)
See downloadable PDF version of the full: CP ITG workstreams.
These sections below set out updates related to these workstreams based on the most recent pharmacy IT bulletin.
Overview of current pharmacy IT priorities
NHS England, the Department of Health and Social Care, and the CP ITG have identified key IT priorities for the pharmacy sector. These include:
- the Professional Record Standards Body (PRSB) Community Pharmacy Data Standard;
- the Community Pharmacy Contractual Framework (CPCF) IT;
- electronic health records;
- service data APIs;
- Booking and Referral Standards (BaRS); and
- the next generation of EPS.
The CP ITG actively supports these projects, with Community Pharmacy England working alongside the NHS to advance these initiatives. These priorities align with the group’s 2025-updated CP ITG’s vision of pharmacy IT and the IT-related aspects outlined in the Nuffield Trust’s Vision for Community Pharmacy. Similarly, the Primary Care Recovery Plan integrates digital elements consistent with these priorities, such as GP Connect Update Record, GP Connect Access Record, and BaRS for pharmacy services.
NHS England continues to work on a framework to incentivise community pharmacy IT system supplier development, aligning with the NHS Community Pharmacy Contractual Framework (CPCF).
An important note was publicly issued by the NHS England National Commercial and Procurement Hub back in August 2025, announcing the market engagement with pharmacy IT suppliers for community pharmacy clinical services IT solutions at:
Community Pharmacy IT Summer 2025 Tender (with the Government’s ‘Find a Tender’ Programme (the usual route for such updates).
Key related dates have been, and are, as follows.
- The market engagement period of seven weeks commenced on 1st September 2025 and this was due to close at 5pm on Monday 20th October 2025 unless of a change announced through the eCommercial System (Atamis) and related communications.
- Interested parties must use the Atamis procurement portal to engage, ask questions and provide feedback throughout the market engagement period.
- The first webinar was held on the 11th September 2025 and provided further information on the market engagement.
Community Pharmacy IT Group has long been supportive of a formal IT workstream route, anticipating that this is a step forward in how IT suppliers can engage with supporting pharmacy owners to deliver NHS services in a more digital and integrated way.
EPS updates: Piloting of prescription readiness notifications
CP ITG pharmacy representatives have long supported the introduction of additional EPS statuses, provided that system design ensures these are easy or automatic to record, keeping the burden on pharmacy teams low. The group has also supported patients receiving relevant updates—such as “ready to collect”—via the NHS App and other apps. Patients themselves have requested this functionality.
Since 2022, the EPS and NHS App teams have been working with EPS system suppliers to enable prescription item readiness information. CP ITG sub-groups have previously discussed this topic. Community Pharmacy England and NHS England have issued news updates to the sector about progress with the National Patient Prescription Tracking Service (NPPTS). Patients have been able to access information within the NHS App about readiness for some time, but NHS App notifications about medicine readiness have not been deployed. The EPS and NHS App teams are now preparing to progress towards an NHS App notification pilot.
Scan-to-shelf
We have received feedback from community pharmacy teams about some potential benefits and challenges with scan-to-shelf technology.
Pharmacy teams and supplier representatives may feedback:
- For those already using scan-to-shelf: what benefits have you seen so far?
- For those not yet using it: what are the main barriers (e.g., cost, equipment, time, process change)?
- What would make it easier for your pharmacy to adopt scan-to-shelf?
EPS IT suppliers have also been provided with an MS Forms survey before the meeting.
Pharmacy teams can send comments to da@cpe.org.uk with any feedback.
Hub and Spoke IT
Background The Government has confirmed that the Hub and Spoke dispensing Model 1 (patient → spoke → hub → spoke → patient) will be permitted from October 2025, following amendments to the Human Medicines Regulations 2012. This will allow different pharmacy businesses to share dispensing processes, provided they have written agreements in place. Key regulatory points:
- The spoke pharmacy remains responsible for supply to the patient.
- Medicines must be labelled with the spoke’s details and the date the hub assembled them.
- Data sharing between hub and spoke is permitted under an information gateway, with confidentiality safeguards.
- NHS spoke pharmacies will need to notify their ICB 28 days before starting hub and spoke for NHS prescriptions.
Community Pharmacy England reported that this month, new hub and spoke dispensing Terms of Service (The National Health Service (Pharmaceutical and Local Pharmaceutical Services) (Miscellaneous Amendments) Regulations 2025) were laid before parliament.
Why IT matters
For hubs and spokes to work effectively, robust digital solutions are essential. These include:
- Interoperability between hub and spoke PMR systems.
- Secure data exchange for prescription and assembly information.
- Workflow visibility for both parties.
- EPS integration, including how single-item prescribing and claim submission will function.
- Automation readiness and barcode scanning processes.
Principles of patient choice of pharmacy within technical tools
The group previously endorsed a set of principles regarding the protection of patients’ right to choose their pharmacy. These principles were focused on EPS prescriptions at the time, but equally fit patients’ right to select a pharmacy to deliver a service. Healthcare providers, as well as IT solution providers, can help to ensure these principles are maintained.
The principles, tweaked to cover pharmacy services, are listed below.
- Patients must be free to select a pharmacy of their choice to dispense their prescription or provide other clinical pharmacy services.
- Patient sign-up for the nomination process or service must be separate and unbundled from any other sign-up procedures. It should also require proactive agreement (not a pre-ticked box).
- Patient information using the NHS logo must not, directly or indirectly, direct a patient’s choice of pharmacy (take a patient’s choice of pharmacy) for dispensing or other pharmacy services.
- Patient information using the NHS logo should follow the NHS England processes for nomination and freedom of patient choice.
- Patient information must follow the NHS (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013 on nominations and the relevant NHS England service specifications.
- Patient information provided by General Practitioners to assist with the choice of pharmacy must include a list of all pharmacies in the area (as provided for in the GP contract) (at least the nearest four, where the most local four is relevant), and inclusion of the current pharmacy nominated for EPS prescriptions, can be included within a list presented to patients.
- Pharmacies (including those using third-party apps) must have the informed consent or agreement of a patient to dispense the patient’s prescription and the provision of pharmacy services.
- Pharmacies must comply with the NHS (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013, specifically, the regulations on the nomination of prescriptions and prescription inducements (including when using third-party apps).
- General practitioners must not seek to persuade a patient to choose to nominate a specific pharmacy (as provided for in the GP contract), including when using third-party apps.
- The NHS logo should be used only following NHS identity guidelines, e.g., only by service providers and not third parties.
- The criteria for NHS-approved technologies, or any similar NHS approval procedure (NHS IM1 integration, NHS GP IT Futures, etc), and continued assured status, should be given/continued only if there is adherence to the above criteria (1-10).
The NHS Constitution guarantees patients’ continued entitlement to fair choice. Service specifications also outline service-specific arrangements to protect patients’ choices of a pharmacy.
Pharmacy IT Priorities
The group’s documents have received more updates since the last meeting:
- Next steps for pharmacy IT (CP ITG) (abridged slides)
- Next steps for pharmacy IT (CP ITG) (full slideset), which has been recently updated to include a full slide each of the group’s workstreams.
The theme across pharmacy requests for IT change, is in line with the 10 Year Health Plan for England, relating to a desire for the ‘seamless flow of clinical information’ (interoperability). A more seamless flow of clinical information would also help to realise Nuffield Trust’s vision for the sector, with it being able to support continuous improvement:
- preventing ill health and supporting wellbeing;
- providing clinical care for patients;
- helping patients to live well with medicines; and
- provision of integrated primary care for neighbourhoods.
The updated ‘Next Steps’ document was shared with NHS England.
The updated table on the next page includes some of the most requested advancements. It does not include all requested items.
Items highlighted in amber are requested as high priority, and those highlighted in red are very high priority. Items highlighted in grey are those being viewed as high priority, but NHS IT advancement to begin for these grey items in the near future, is not yet confirmed.
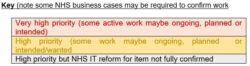
Pharmacy representatives’ views on
pharmacy NHS IT priorities
The group supports all future workstreams in the table being incorporated into future rounds of NHS Digital Services for Integrated Care (DSIC) pharmacy IT programme.

Pharmacy teams can send additional comments to da@cpe@org.uk with any feedback.
Pharmacy First IT
NHS England and its Transformation Directorate are continuing to work with four IT system suppliers to ensure the remaining Pharmacy First functionalities:
Previously, the system suppliers updated their NHS-assured IT support for the Community Pharmacist Consultation Service (CPCS) to incorporate the additional elements of the Pharmacy First service. As a result, pharmacy owners continue to have the option to either:
- Continue using their current IT system supplier for Pharmacy First IT support or
- Transition to another NHS-assured Pharmacy First IT system supplier.
NHS Community Pharmacy Contractual Framework (CPCF) pharmacy IT
- NHS England and Community Pharmacy England have expressed the need for suppliers to receive comprehensive information about the service, including the IT implications and dataset requirements. The minutes and slides from the group’s previous meeting provide further details on the progress of MYS APIs. The MYS API priorities were previously listed as Pharmacy Contraception Service, Discharge Medicine Service (DMS), Blood Pressure Checking Service, New Medicines Service (NMS) and Smoking Cessation Service. CP ITG pharmacy representatives previously reported that data entry for services like DMS consumes excessive time for many pharmacy teams. In response, NHSBSA previously issued an expression of interest for the DMS API to assess the market’s interest in providing this integration service. Both NHS England and NHSBSA remain committed to prioritising the progress of the API programme.
Artificial Intelligence (AI) governance
- NHS Confederation published a report on Artificial Intelligence use in NHS communications: insights, risks and recommendations for safe and effective adoption of AI in NHS communications.
- Tony Blair Institute for Global Change published an article, Sovereignty, security, scale: a UK strategy for AI infrastructure.
- The Lead Pharmacist at West London NHS Trust emphasised the need to act fast to close the NHS AI safety gap.
Artificial Intelligence (AI) and health
- NHS Confederation published a report, Scaling AI in healthcare.
- The Telegraph published an article on How AI could save the broken NHS.
- BMJ published an article, NHS 10 year plan: can using AI offer a solution to the NHS’ problems?
- Nature published an article Beyond AlphaFold: how AI is decoding the grammar of the genome.
- Pulse opined on how NHS could resist the urge to replace GPs with AI.
- Mercer published an article on Transforming the healthcare workforce with AI.
Standards and interoperability
- Community Pharmacy England reported on GP Connect: Update Record developments.
Updating the SNOMED CT UK Drug Extension model to reflect the SNOMED International model for national drug extensions
NHS England provided an update to the July announcement regarding Phase 1 of the planned changes to the SNOMED CT UK Drug Extension.
NHS England will implement these changes in release 41.0.0 on 1 October 2025.
For more details, please visit the NHS England webpage.
System suppliers, pharmacies or other CP ITG participants with questions or who would like to discuss this work further, contact: nhsdigital.ukmeds@nhs.net.
Independent prescribing IT
The General Pharmaceutical Council (GPhC) previously consulted and reported on changes to the requirements for entry to independent prescribing courses. The Pharmaceutical Journal reported that independent prescribing piloting was to begin across England. NHS England continues to advance independent pharmacy prescribing through the Community Pharmacy Independent Prescribing Pathfinder Programme. Pathfinder sites were previously selected to implement prescribing models in three categories: existing community pharmacy services, long-term conditions, and novel services. CLEO SOLO is assured for use by sites, continuing to enable community pharmacists to generate prescriptions via the Electronic Prescription Service (EPS). CLEO SOLO is currently the sole supplier in the community pharmacy IP EPS space.
Other NHS account and NHS App updates
- Community pharmacy teams are invited to take part in a new Autumn 2025 NHS England pilot aimed at improving the prescription tracking experience for patients using the NHS App to hear about medicines readiness through NHS App. The group’s pharmacy reps are encouraged to all take part.
- Community Pharmacy England reported Rollout of prescription status info in the NHS App continues.
- NHS England published the NHS App test results promotional toolkit which promotes how patients can view test results that have been added to their the NHS App ‘health record’ information section.
- DHSC announced Patients in England will receive appointment reminders, screening invitations and test results through the NHS App first, as part of a £50 million upgrade.
- DHSC announced NHS App feature will enable patients to sign-up for clinical trial.
- The Prime Minister announced that People diagnosed with long-term health conditions will receive extra help and support from charities via the NHS App.
- NHS England published its latest NHS App roadmap. Recent updates include visual graphs for hundreds of test results, helping patients track their health trends.
Patient digital tools and apps: case studies
- The NHS England social media team has launched an official NHS WhatsApp Channel, designed to get trusted health information straight to the public’s phones.
Records: National
- UKAuthority reported that A single patient record for the NHS should include an audit trail to show who had accessed the data, according to the views of patients involved in discussions on the concept.
- Chief Medical Officer for Alcidion, considered how emerging policy could help patient record systems to become more active and intelligent, enhancing the delivery of care.
Genomics
- Genomics Education Programme published Pharmacy personas to support genomics-informed medicines optimisation.
- Community Pharmacy England reported that the Cybersecurity Unit at DHSC launched a pilot study to explore the benefits of enhanced cybersecurity support for community pharmacies. The pilot group has met and is able to use an National Cyber Security Centre (NCSC) cyber security beta tool and use a unique pilot link to support lessons from the pharmacy and healthcare use of this tool.
Urgent: Action required by IT suppliers and IT support teams to support the ongoing use of the Care Identity Service
The NHS Care Identity Service (CIS) team has published IT teams need to update to the latest version of Identity Agent – Outages for TLS 1.0 and 1.1 – updated schedule. In line with stopping the use of deprecated TLS, Care Identity Service will begin a phased approach to blocking traffic to CIS1 Authentication where deprecated TLS (1.0 / 1.1) is detected. The next announced phased blocking periods: Mondays 22nd and 29th September, from 15:00 to 16:00 (1 hour each day).
Deprecated TLS will be permanently blocked from use in CIS1 Authentication on Wednesday 15th October at 15:00. Users of applications using CIS1 Authentication and CIS2 Authentication and unsupported version of Identity Agent may see a message warning them that their locally installed software is unsupported. This may also be relevant to larger pharmacy organisations that manage branch environments, including Smartcard software on machines. Read more.
IT policy: priorities, reports and the future
- Community pharmacy England reported that NHS England launched a new community pharmacy Point of Care IT Supplier Contractual Framework.
- Community Pharmacy England reported on The Government is advising community pharmacy owners to take action to prepare for the upcoming national switch-off of the Public Switched Telephone Network (PSTN), which is due to be fully decommissioned by January 2027.
- The Public Policy Projects published a report on Maximising the impact of the NHS federated data platform.
- NHS Providers published a report on Digital transformation and the productivity and efficiency challenge.
- Health Business reported that the NHS is accelerating its digital transformation to improve patient care amid rising pressures on staff, budgets, and resources.
- Chancellor Rachel Reeves announced that the government will invest up to £10bn in NHS tech “to bring our analogue health system into the digital age”, as part of the latest spending review.
- The Guardian reported that Wes Streeting staked the future of the NHS on a digital overhaul in which NHS App and new hospital league tables are intended to give patients unprecedented control over their care.
- Genomic data and expansion of the NHS App are central to the government’s 10 year plan for a Neighbourhood Health Service.
- Tony Blair Institute for Global Change published an article The NHS at a crossroads: the NHS App that can transform Britain’s health.
- NHS digital leaders welcomed the 10-year health plan for putting digital and data “front and centre” of the government’s drive to transform the health service, but warned that a huge piece of work on delivery is required to fill in the missing detail, unpick “contradictions” and support the digital workforce.
- NHS England issued a procurement notice for a £154.8 million contract to support greater “personalisation” of digital services and help deliver service upgrades.
- A panel of experts identified the lack of standardised data as a key barrier to the government’s digital health plans.
- The NHS Confederation published an article, Delivering a neighbourhood health service: what the 10 Year Health Plan means for local integration.
IT policies: localities, organisations and suppliers
- NHS England published the Tech Innovation Framework which supports system suppliers as they work to deliver cloud-based, innovative clinical products into the GP marketplace.
- NHS England published the primary care service development funding and general practice IT funding guidance 2025/26. It is designed to help ICBs understand the changes for the year and support them in making informed decisions about how they will use the funding.
- The High Impact Change Model is designed to support local health and social care system leaders to work together to embed and improve data-driven decision making at all levels, resulting in the delivery of better neighbourhood health outcomes.
- NHS England approved the first of a new generation of electronic patient record systems for GP teams – with more suppliers expected to be made available later this year.
- NHS England reported that Microsoft announced that free support for Windows 10 will cease in October 2025. After this date, Microsoft will no longer provide free updates, including security patches, for Windows 10 systems.
- NHS Providers published an article Mastering NHS supplier relationships for a digital NHS.
IT policy: commentary and requests for the future
- Tech World published an article, Is the 10 Year Health Plan really fit for the future?
- The Conversation opined Overhauling the NHS App is at the heart of UK healthcare plans, but it could leave some people behind.
- The Health Foundation expressed views on 10 Year Health Plan – ‘we need to move from ‘techno optimism’ to techno realism’.
Digital inclusion
- NHS England is introducing changes to Reasonable Adjustment Patient Flags.
This involves asking local IT suppliers to read the Developer Catalogue – Patient Flags and register their interest to begin onboarding the Patient Flag API register.
- NHS England’s Transformation Directorate’s BaRS programme continues to aim to enable booking and referral information to be sent between NHS service providers in a format that is helpful to clinicians. The intention is for BaRS to eventually be available in all care settings. The minutes and slides from the group’s previous meetings contain additional information about BaRS and pharmacy use cases. CP ITG feedback indicated that the BaRS programme should be expanded to incorporate NHS appointment standards.
- Pharmacy teams can provide updates about any efforts to move towards more paperless work by contacting it@cpe.org.uk.
See: CP ITG workstream updates (archive) for older updates in html format. The bulletins (including the most recent one) can also be downloaded in pdf format at the CP ITG webpage.
Get involved
If you have a related query or would like to feed into the CP ITG or share your updates about IT and digital issues then please don’t hesitate to contact one of the group’s organisers, Dan Ah-Thion or it@cpe.org.uk or you can also sign-up to join the virtual Community Pharmacy Digital Group which helps inform CP ITG’s work with others. You can be involved as much or as little as you like with CPDG, and can unsubscribe from that email group at any time.
Return to the Pharmacy IT hub; CP ITG; Get involved; IT policy or IT a-z index
For more information on this topic please email it@cpe.org.uk