Enhancing EPS or preparing for it
Published on: 16th July 2013 | Updated on: 7th April 2022
 EPS enhancement and preparation info is set out on this webpage.
EPS enhancement and preparation info is set out on this webpage.
Click on a heading or link to ‘show’ or read more or return to EPS home for more on EPS.
To get the most out of EPS, refer to the EPS essential checklists.
To obtain the full benefit from EPS and minimise disruptions, pharmacy staff need to be trained in how to use the system. Where training has been inadequate, or not taken up, there have been cases where problems have emerged as a consequence.
Whilst system suppliers are responsible for delivering training in the use of systems, pharmacy contractors are responsible for working with suppliers to ensure that training is sufficient and meets the needs of individual staff. The following list of tips to consider when organising training has been compiled from feedback on experiences to date.
Plan training in advance
- Planning is a must – set out a plan with a rough staff availability/training timetable outlining.
- All staff included: Make provision for part-time staff and locums. E.g. designating a member of the pharmacy team to train part-time workers.
- There will be different training needs for different staff. E.g. counter staff may need to understand nomination but not how to claiming.
- Vital messages missed if training missed: In some of the cases where problems have arisen to date, pharmacy staff were offered training but chose not to take it because they initially felt that use of the system seemed intuitive.
EPS training sessions
NHS Digital conducted more than 800 EPS training sessions across the country throughout England during 2015-16. The training events were organized in association with PMR dispensing system suppliers, Local Pharmaceutical Committees (LPCs), and NHSBSA, to help all pharmacy staff including: counter staff, dispensing technicians, pharmacists and locums to get the most out of EPS. The free training focused on three areas: PMR training, business process and submission. Although those events have completed, PMR suppliers continue to make training options available.
Training timing options
- Time training close to GP go-live: If training is delivered too early (e.g. more than a few days) key messages can be forgotten. Many pharmacies have found that a few hours prior to go live is the best time to deliver training to pharmacy staff.
- Second stage of training once pharmacy receives more R2 prescriptions: If the pharmacy is going-live well in advance of receiving R2 prescriptions, consider delivering training in two stages: (1) basic training on the go-live day (2) in-depth training at the point that the pharmacy starts receiving electronic prescriptions.
- Capture nomination in advance: Where pharmacy teams have captured large volumes of nominations prior to a local surgery going live, this has enabled staff to cement business process change early. Where low numbers of nominations are recorded, the re-education of staff to new processes has been slower. If there is a delay of greater than four to six weeks between adjusting on the Personal Demographics Service, then re-confirm nomination in case they have selected another dispenser.
- Use quiet periods for training: E.g. when the pharmacy is closed or when there is locum cover. This will allow staff to concentrate fully.
Training options
- System supplier training: Find out what type is offered. E.g. one to one staff training, webinars, training videos, user manuals, quick reference guides and/or desk aids and help files on the system. A list of options available has been published on the NHS Digital Website.
- Read system supplier information: Make sure that you take time to read any information packs you receive from your supplier as these could contain links to manuals, videos or dates of Webinar sessions.
- Use e-learning: If the supplier offers this, ensure that dispensary computers can run the e-learning module – including playing any videos and sound.
Training for business optimisation
- Meet with local GP practices to agree changes to processes will help smooth implementation. In some areas, local NHS England teams organised workshops or awareness sessions to support discussions on business change.
- Adapt existing business processes: To maximise the benefits. Explain the changes to staff.
- Train locums with the process: Whilst locums might be familiar with the system, business processes are unique to each pharmacy.
- Configurations adjusted to suit you: During system setup, ask for the system to be configured to suit your business processes. Spend time checking optional configurations to the system to meet your needs.
Post-Training support
- Dealing with system issues: All staff should be made aware of the helpdesk process for system issues and keep the contact details visible in the event of any issues.
- Consider scheduling a brief weekly troubleshooting session: This gives staff an opportunity to talk to each other, discuss new ways of working and make suggestions on how new processes can be optimised.
If a supplier has delivered training but the training methods or materials have not been sufficiently comprehensive, it is essential to let both the supplier know, so that improvements can be made.
| Top tip | Summary | Advice |
| Staff support | Having staff more knowledgeable on the topic can reduce the risk of problems. | Assign an EPS lead within the pharmacy team to help other staff: A successful approach to implementation was the appointment of an in-store ‘pharmacy champion’ to provide first line support to other pharmacy staff during deployment of EPS R2. |
| Training | Ensuring relevant staff are fully trained and comfortable with EPS can ensure a smoother transition and correct reimbursement. |
A range of info and factsheets are at: https://cpe.org.uk/eps Also see below the table for info about PMR supplier training.
|
PMR suppliers are offering are a range of training methods and materials. Their website and contact info is at: https://cpe.org.uk/supplierlist
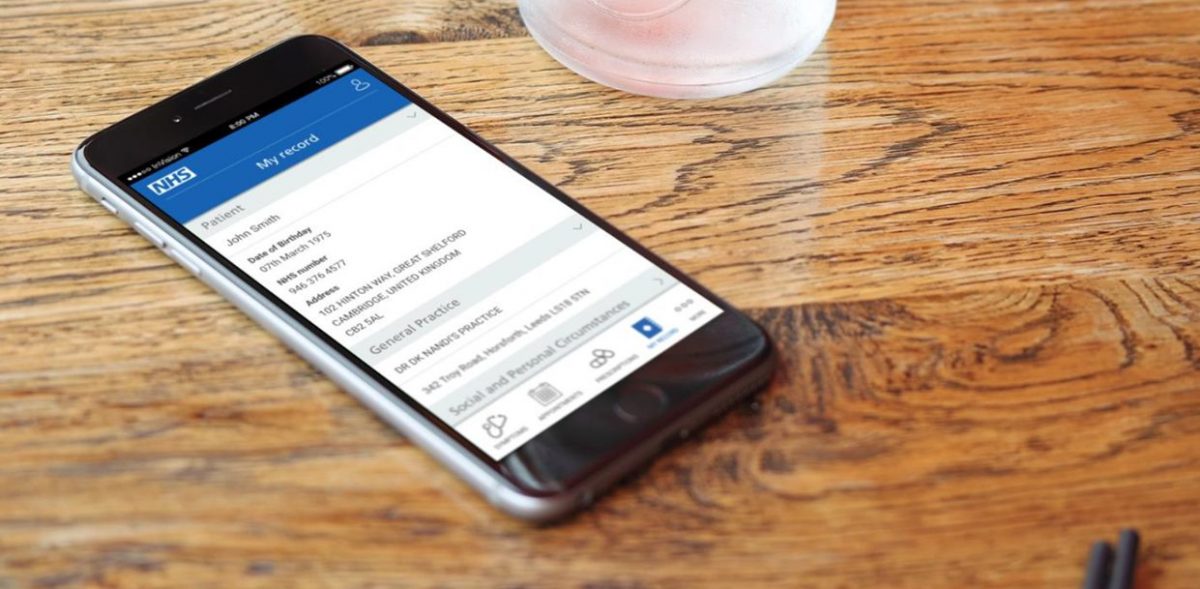
Regulations state* that contractors must explain Electronic Prescription Service Release 2 (EPS R2) to patients,
- whether or not EPS is available at that pharmacy.
- when it EPS is not available at the pharmacy, the pharmacist where they know, shall provide the patient with contact details of at least two nearby EPS R2-enabled pharmacies.
Read more: Nomination.
*National Health Service (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013
Patient information leaflet
A leaflet may help you explain EPS for patients. There are nationally developed leaflets such as:
- a Community Pharmacy England leaflet using NHS Digital suggested text can also be found here.
Patient video
Patients can be introduced to the service via a 90 second EPS patient video. The video is available to display on digital screens in waiting areas or on pharmacy websites.
Developing your own EPS R2 communications
NHS Digital previously consented to the nationally produced patient information sheet being used as a template for local adaption. For locally produced EPS communication materials, pharmacies need to take care to ensure compliance with the NHS Brand guidelines if planning to use the NHS logo and the EPS Release 2 Design Style Guide if planning to use the EPS Release 2 device.
As part of the EPS Release 2 design style requirements, pharmacies should only use the EPS Release 2 device in promotional material if they are either operating or due to start operating EPS R2.
The NHS (Pharmaceutical and Local Pharmaceutical Services) Regulations 2013 require pharmacies to acknowledge in advertising material that NHS Essential and Advanced services are funded by the NHS – this requirement encompasses EPS.
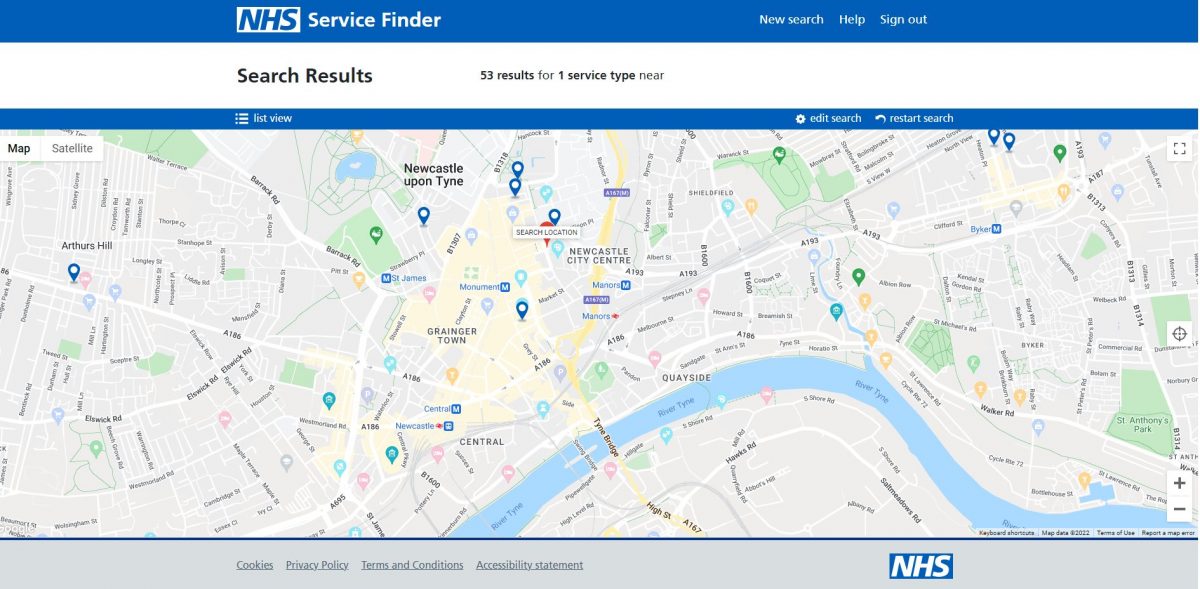
It is important for pharmacies to be aware when local GPs are going live with EPS R2
GPs requirements before they ‘go live’ with R2
To go live with R2, GP practices must have:
- An adequate system: access to a R2-enabled GP system (‘full roll-out authority’, a list of these can be viewed here).
- Local NHS England team approved application form: an application form submitted to the relevant team to approve. The application can be submitted by the GP practice, the GP’s CCG or by the GP’s local support organisation responsible for providing GP IT support services on behalf of the CCG (e.g. CSU or Health Informatics Service).
8-week process for GPs going live
To ensure dispensers are given enough notice of applications should be submitted at least 8 weeks before a proposed ‘go-live’ date. This allows local pharmacies affected by a deployment to obtain tokens and working smartcards. The applicant applying for the GP to go live must confirm on their application form that relevant LPCs have been engaged as part of the deployment process. The local NHS England team will reject the application if one or more of the following reasons apply:
- The proposed go-live date provides less than 8-weeks’ notice;
- The applicant has not confirmed that relevant LPCs have been engaged or;
- Smartcards and dispensing tokens (FP10DTs) are not available for all nearby pharmacies.
Without approval from the local NHS England team, the GP practice will be unable to obtain an ‘end point’ (the central technical switch allowing R2 at that site).
The process will enable a GP practice to go-live for up to two weeks after the planned date. However, if an R2 prescription has not been issued by this time, the ‘end point’ will be removed and another application must be made, ensuring that there is again 8-weeks’ notice for a newly proposed date.
Planned deployment information can be reached online using updated NHS Digital resources; the deployment map or via a downloadable Excel list can be found there.
NHS Digital contacts LPCs each week providing details of pharmacies in a locality that may be affected by planned go-lives.
Business change workshop
Attending local business change workshops can help pharmacy teams and GP practice staff get to grips with EPS before the GP ‘goes live’ with the system.
Learn more in this NHS Digital produced factsheet:
Related resources
One of the key lessons has been that good communication and understanding between GP practices and pharmacy teams is essential to ensure smooth introduction and running of EPS.
In some areas, immediately following deployment, pharmacy teams and local GP practice:
- identified named contacts for dealing with queries and ensuring regular two way communication; and then
- booked a series of weekly 10 minute catch-up meetings to review problems that have arisen in the previous 7-days (via face-to-face meetings or pre-booked telephone calls).
Of course pharmacy teams will dispense prescriptions from multiple GP Practices and this can be considered when planning a local engagement strategy.
Another approach tried is the exchange of updated SOPs relating to key processes such as repeat prescription ordering. There is scope for LPCs and LMCs to work jointly to facilitate local dialogue, for example arranging an event for GP Practices and pharmacies in the locality to meet jointly.
GP-Pharmacy engagement checklists
Use the checklists below to ensure GPs and pharmacies know how to work with each other
(for example how to work if there is internet failure at the pharmacy, and how to deal with patients on a mixture of paper and electronic)
- How GPs and pharmacies can work together on EPS business continuity (2017)
- EPS pharmacy and GP checklist – working together (2017)
Previous NHS Digital checklists from 2012 are listed below:
These were developed with input from GPs and pharmacists that have recently deployed the service, which has been designed to support local inter-professional discussions before, during and after go-live.
Read more at:
- Changing PMR (system supplier);
- Choosing connectivity (HSCN/N3);
- Getting Smartcards & setting card admins;
- Setting EPS nominations, Preparing EPS contingencies;
- Getting EPS tokens
Q. I’m a newly opened pharmacy and will be upgrading my PMR system from Release 1 capable to Release capability?
Consider the information set out within: Upgrading EPS from Release 1 to 2
Further info
If you have queries on this webpage or you require more information please contact it@cpe.org.uk. To share and hear views about digital developments with like-minded pharmacy team members, join the CP Digital email group today.
Return to the Pharmacy IT hub; EPS home or IT a-z index