Submission (EPS)
Published on: 16th July 2013 | Updated on: 19th November 2025
EPS endorsing, submission and reconciliation info is set out on this webpage.
Click on a heading or link to ‘show’ or read more or return to EPS home or EPS dispensing for more on EPS.
EPS Serious Shortage Protocols (SSPs)
The June 2021 Drug Tariff introduced changes to endorsing requirements for Serious Shortage Protocols (SSP). It readied contractors for an improved EPS endorsement and transition away from use of NCSO and towards using ‘SSP’ instead if pharmacy contractors will wish to confirm SSP processes were used.
For SSP dispensing with EPS, previously the quick introduction of SSPs back in 2019 meant that system suppliers were requested to use a workaround in which the NCSO endorsement field was used instead of a brand new endorsement option.
Pharmacy contractors had fed back to Community Pharmacy England that they supported a proper electronic solution. NHSBSA and PMR suppliers have been working towards this with support from DHSC and Community Pharmacy England.
The June 2021 Drug Tariff introduced changes: The SSP EPS endorsement should be used once PMR suppliers have made new endorsement available. PMR suppliers have been asked to introduce the function as soon as possible and most have already done so.
Contractors endorsing that an SSP item was issued are recommended to use the SSP endorsement.
It was communicated that a limited transition period in which the older endorsement can be used would take place until the end of September 2021, but it was recommended from mid-2021 for contractors to get in the habit of endorsing SSP now to prevent risk of reimbursement loss later. Any SSP claims after the transition period made using EPS tokens will no longer be accepted for payment.
Suppliers also have some flexibility as to the extent to which they will support pharmacy team members for example, by asking users to complete any missing or incomplete SSP endorsement information if the required endorsements are not present or not in the specified format. Some suppliers will be able to prevent the EPS SSP endorsement being submitted if certain information is not populated as expected (e.g. an up-to-date and accurate SSP number and an SSP number in the right format).
It is recommended
PMR specific guidance links and other EPS information can be found at the Community Pharmacy England SSPs webpage.
Information required by the Pricing Authority to price prescriptions
The information required to be sent to the Pricing Authority electronically is, as now, only the essential information required to price prescriptions. Information on the dispensed product, where required, will be provided to the Pricing Authority using the dm+d code for the product.
Other endorsements will also be required, in the same way as now, for example endorsements to claim broken bulk or out of pocket expenses or the NCSO concession. Pharmacy systems will support pharmacy staff in making these endorsements electronically.
Useful resources:
Some pharmacy contractors currently make endorsements manually by hand without any support from their pharmacy systems. In these cases, pharmacy staff will in future be required to use their pharmacy system to make endorsements electronically.
| Product Type Prescribed | Information Required by the Pricing Authority |
| Generic Product listed in Part VIII of the Drug Tariff | VMPP or ‘nothing’* |
| Generic Product which is not listed in Part VIII of the Drug Tariff | AMPP or AMP |
| Branded product | AMPP or ‘nothing’* |
| Appliance prescribed generically and only listed generically in the Tariff (e.g. Absorbent Lint BPC) | VMPP or ‘nothing’* |
| Appliance prescribed generically but listed by Brand name in the Tariff | AMPP, AMP or ‘nothing’* |
| Appliance prescribed by Brand Name(but listed generically in Tariff) | AMPP or VMPP of the dispensed item, or AMP or ‘nothing’* |
*When the dispenser submits ‘nothing’ in the reimbursement claim message, the pharmacy system will default to the dm+d code for the prescribed item.
Endorsement information required
Community Pharmacy England and NHSBSA are receiving more contractor queries about EPS prescriptions endorsed without the necessary product and pack size information for drugs not listed in Part VIII of the Drug Tariff. This follows an increase with EPS usage which has occurred over the course of the pandemic.
EPS prescriptions submitted without the necessary information lead to prescription returns (referred backs) and delays in payment.
The most common reason for EPS prescription returns is where the prescription was for a non-Part VIII product and the prescription hasn’t been endorsed with a required invoice price e.g. for less common items for which NHSBSA holds no price.
When dispensing a drug that is not listed in Part VIII of the Drug Tariff, contractors are reminded the EPS message must include:
- the quantity dispensed (if different to the quantity prescribed)
- the pack size used; and
- the brand name or name of the manufacturer or wholesaler from whom the supply was purchased (if the order is in the ‘generic’ or pharmacopeial form).
Much or all this information may be automatically added by your confirmation of the actual medicinal product pack (AMPP) which was dispensed. The process for submitting this information using different PMR systems can vary. Your PMR website or PMR help/guidance documents can also assist you.
Some PMR suppliers have added prompts so that users will add all information required by the NHSBSA. Such prompts may reduce the number of EPS returns you’ll receive. Read more about providing feedback to your supplier at: cpe.org.uk/reportIT.
Endorsing non-Part VIII EPS items
Some example scenarios for EPS endorsing when: NHSBSA hold a price, a price endorsement is required or the AMPP cannot be selected:
1. Endorsing by selection of AMPP (if a price held by NHSBSA)
Your PMR may enable you to add the relevant information to the EPS message by selecting the AMPP which you dispensed.
NHSBSA will price using the dm+d reimbursement price, regardless of whether an invoice price is endorsed.
Contractors should ensure that the correct AMPP is selected as dispensed, as endorsement of the wrong product or pack size could result in reimbursement for a product different to what was originally supplied. For example, if you inadvertently endorse the first entry in the ‘pick list’ you will be reimbursed for that product, even if you dispense a different product at a different price.
2. Endorsing Invoice Price (IP) (if no price held by NHSBSA)
For those non-Part VIII items which NHSBSA holds no price, the endorsement should also include the pack size Invoice Price (IP)
This enables NHSBSA to calculate the overall price even if you have supplied a quantity different from a complete pack. When adding an invoice price endorsement to an AMPP, contractors should ensure that both match the pack size supplied.
3. AMPP not listed on dm+d
If a product or pack size dispensed is not listed in dm+d, contractors should return the prescribed product (the generically prescribed virtual medicinal product (VMP)) and an invoice price endorsement including price, pack size and supplier details.
On occasion, products may be listed on dm+d but not updated on PMR systems. This could prevent users from being able to select and dispense an AMPP. If there is a dm+d mapping or listing error, contractors should follow reporting process outlined at the dm+d webpage.
For more about the new ‘FS’ endorsement, see the section below.
Exemption factsheet
Read our EPS exemption factsheet
Prescription charge/exemption status
In addition to the current endorsing information, pharmacy staff will also have to mark whether a prescription charge was levied for a prescription, and where relevant the prescription charge exemption category and whether evidence of exemption was seen. The exception to this is where the patient is age exempt and the patient’s date of birth is included in the electronic prescription message. For EPS prescriptions, systems may compare the date of birth with the date of the dispense notification to determine whether age exemption automatically will apply. If the declaration date takes place at a different time, systems can allow the pharmacy to determine age exemption manually.
Old patient charge rate and new charge rate
Any paid electronic prescriptions dispensed in a financial year by end of March with an NHS prescription charge levied at the charge rate for that year. If the charge rate increases the following year (as is the case for previous years) this will impact charge deductions. Regarding EPS: if the Dispense Notification (DN) message is submitted before 31st March and the corresponding Claim Notification or Electronic Reimbursement Endorsement Message (EREM) is received by the NHSBSA by the end of 5th April 2021. Please see below how paid electronic prescriptions are treated by the NHSBSA following a change to the prescription charge rate.
- If a DN is submitted on 31st March and EREM is received by NHSBSA by 5th April – this would be treated as March dispensing (charge rate which applied within March – ‘old rate’)
- If a DN is submitted on 1st April and EREM is received by NHSBSA by 5th April – this would be treated as April dispensing (‘new rate’ which applies for April and onwards)
- If a DN is submitted on 31st March and EREM is received by NHSBSA on or after 6th April – this would be treated as April dispensing (‘new rate’ which applies for April and onwards). There would be no checking of the dispense date in this instance as the claim message was submitted would be outside of the first five days of the following month (EPS 5-day window).
Pharmacy system supplier enhancements to ease data input
Pharmacy system suppliers have flexibility in the way that they develop systems to support pharmacy staff in entering this information. Different systems provide different levels of support to pharmacies. This is a key area for pharmacy contractors to engage with suppliers to ensure that systems meet user needs, for example:
If exemption information hasn’t been recorded in the local system, does your system automatically default to recording electronic prescriptions as ‘paid’ or before allowing a message to be sent for payment, does your system always prompt staff to confirm the prescription’s exemption status to ensure that this is entered correctly?
- If pharmacy staff have already recorded details of a valid exemption certificate in the PMR system, for example a pre-payment certificate, the system could be set to pre-populate this information in the electronic reimbursement claim message, reducing workload. Note, the pharmacy would still be required to collect the patient’s exemption declaration on the prescription or dispensing token, where required.
- Where a system supports auto-population of exemption information, are there controls to ensure that when an exemption certificate expires, pharmacy staff are prompted to check whether the patient remains exempt and input up-to-date information, as appropriate?
- Is there a management screen or system report that allows, at a glance, a sense check that exemption information has been input by staff where required?
Pharmacy systems may need to carefully consider how to count EPS contraceptive items, e.g. as ‘paid no charge’ in order so that this reconciles with how NHSBSA will count these.
Guidance on other areas where pharmacy contractors have reported differences between PMR systems in the usability of the EPS R2 functionality can be found in the PMR Suppliers section of this website.
Free-of-charge (FOC) statuses
Free-of-charge statuses can apply to certain types of EPS items. The status applies to item level. Prescribers have been asked to prescribe FOC items onto separate prescriptions to simplify the processes for patients and pharmacy teams.
If EPS prescriptions include an FOC item and a non-FOC item, the FOC status applies only to the FOC item and not the EPS prescription.
Contraceptive items with relevant criteria fulfilled are an example of EPS items with FOC status.
Contraceptive FOC status
Whilst category X was removed from the reverse of the new FP10 forms and Tokens, the EPS message code ‘X’ (0010) for “was prescribed free-of-charge contraceptives” will remain on EPS systems that usually display it. This message code remains on EPS systems because population of a message code field is mandatory before an EPS claim is submitted for payment to the NHSBSA.
Contraceptive FAQ. I received an electronic prescription for a contraceptive. The prescription was incorrectly marked as ‘paid’ when the reimbursement claim was sent. Will a charge be deducted during prescription pricing?
A. Prescriptions for products listed in the ‘No Charge Contraceptives’ section of Part XVI of the Drug Tariff, prescriptions for contraceptive devices listed in Part IXA of the Drug Tariff, spermicidal gels, creams, films and aerosols are automatically exempt from the prescription charge. As with paper prescriptions, even if the claim is marked as ‘paid’, no charge will be deducted for these items.
Electronic prescriptions for other drugs will also be exempt from the prescription charge if the prescriber has made the endorsement ‘CC’ in the prescriber endorsement field in the electronic message. Even if the prescription has been marked as ‘paid’ by the pharmacy, no charge will be deducted if the ‘CC’ endorsement has been made in the prescriber endorsement field.
There is no exception from the requirement to obtain a completed exemption declaration on the grounds that the patient has been prescribed a contraceptive.
EPS scripts with FOC plus non-FOC items
Ideally, prescribers should not include EPS items classed as FOC on the same EPS prescription form as a chargeable item.
DHSC guidance states that “free-of-charge items should not be included on the same prescription form as items for which a charge is usually applicable”. NHSBSA’s “Requirements and Guidance for Endorsement in the EPS” also states “prescribing systems should assist prescribers by splitting items onto separate prescriptions where a combination of [FOC such as contraceptives] and other chargeable medication items are prescribed at the same time”. Where prescribing systems have not been updated, it may be technically possible for pharmacy teams to receive EPS prescriptions with both FOC items (e.g. contraceptives) and chargeable items despite this guidance.
There may be a risk of an incorrect number of prescription charge deductions being made against such prescriptions based on the category selection made via the EPS submission for entitlement to free prescriptions. For example, if an EPS prescription includes a FOC contraceptive and another chargeable item, and the prescription is submitted with the “was prescribed free-of-charge contraceptives” message code ‘X’ (0010) applied to the EPS message, a charge deduction will apply to the chargeable item even if the patient was exempt from prescription charges for other reasons, for e.g. medical exemption. An EPS prescription of this type should have been submitted with actual exemption reason which is applied at a form level rather than the item-level, “was prescribed free-of-charge contraceptives” reason for entitlement to free prescriptions.
Some PMR systems may auto-populate the required EPS message code in the appropriate way to simplify pharmacy processes. PMR systems may also provide support to minimise the risk of pharmacy staff making incorrect category or EPS message code selection errors which may result in inappropriate charge deductions (for e.g. by preventing selection of the ‘contraceptive’ status to the whole prescription if other chargeable items are ordered on the same prescription).
Community Pharmacy IT Group, Community Pharmacy England and NHS Digital have flagged these issues with all the PMR suppliers. You may contact your PMR system if you’d like to see further improvements in relation to the system’s ability to support your processing of FS endorsed prescriptions. PMR suppliers make changes primarily based on the direct feedback they receive.
Read more about making suggestions and feeding back to your PMR supplier at: cpe.org.uk/reportIT.
Free supply (FS) FOC status
The ‘free supply of health treatment’ (FS) endorsement can be made by the prescriber if their prescribing system allows. FS applies to specific reasoning:
| FS reasoning allowed | Anticipated volumes within community pharmacy |
| Sexually transmitted item (STI). | May appear within some community pharmacies |
| Tuberculosis (TB) (since 1st December 2025) | |
| Other reasoning may be specified as required, and in alignment with charges regulations. | N/A |
As with other FOC items, such as contraceptives, there is no patient tick box on the paper FP10 form and Token. This is because legislation does not require a patient, or their representative, to make a declaration or sign a form to receive FOC items. Patients are not required to provide evidence of entitlement for FS FOC treatment. In EPS, however, a new message code for “was prescribed free-of-charge for specified treatment” was added to dispensing systems for scenarios where the prescriber has endorsed ‘FS’. For prescriptions which only have FS endorsed items, the message code 0017 will need to be populated before an EPS claim is submitted for payment (some PMR systems may apply this code automatically if an FS endorsed item is prescribed).
In late 2025 EPS IT suppliers were advised to re-label the message within EPS IT systems given the addition of Tuberculosis (TB) (which applied for 1st December 2025 onwards).
If the FS endorsement is not working at a GP practice but they wish to make use of the endorsement, the prescriber should revert to issuing a paper prescriptions with FS manually endorsed next to each item required.
See further information in the EPS dispensing ‘Dosage area’ section and also at Avoiding EPS product info in dose area factsheet (Community Pharmacy England pdf one-pager) and cpe.org.uk/dosearea.
During the dispensing process pharmacy staff will need to submit a ‘reimbursement claim message’ to the Pricing Authority which includes endorsement information and information on the prescription charge status of the prescription. This can be done either at the same time as sending the ‘dispensed notification message’ or separately at a later date. More information can be found in the endorsing and submission section.
Sending messages regularly can reduce adverse impact in the event that you experience a PMR system crash and need to revert to a past back-up of those prescription listed on your system.
Q. Will the Pricing Authority (PA) allow me to amend a prescription after I have already sent it to them for pricing?
A. A paper prescription cannot be amended after the PA has received it for pricing.
However with electronic prescriptions, it may be possible to make a change (such as amending an incorrect endorsement or adjusting the patient exemption category) after the prescription claim message has been sent to the PA. This is subject to the following criteria:
- your PMR system supplier must have added the functionality required to recall claim messages,
- it must be before the deadline of the 5th day of the month following that in which supply was made.
After this time the PA’s pricing process will begin and the prescription can no longer be recalled.
If these criteria are met, your PMR system can allow you to recall, correct, and then resend the electronic script to PA.
System suppliers which have not already, can choose to set up the ‘claim acknowledgement’ feature. This confirms within your PMR those claims which were submitted and received by NHSBSA. This can provide reassurance that faults have not prevented messages from being sent to NHSBSA via the central NHS Spine.
This feature is included on the PMR wishlist. PMR suppliers make developments partially based on the ongoing feedback they get from their pharmacy customers. Read more at: https://cpe.org.uk/systemlist
See: Submitting in time
Pricing Authority Resolving Issues: EPS returns
In some scenarios, the Pricing Authority return prescriptions to pharmacy contractors where there is insufficient information on the prescription form to process the prescription. Pricing Authority staff may contact pharmacies by telephone to try and resolve issues that arise.
FAQs: EPS returns
Q. I dispensed an electronic prescription for a non-Part VIII generic last month. NHS Prescription Services Pricing Authority have returned and asked about the invoice price for the dispensed product. Why have they done this?
A. Where NHSBSA have insufficient information to process an electronic prescription, this will be returned. Early indications are that compared to paper prescriptions, significantly fewer items on electronic prescriptions require clarification. The most common reason for pharmacies to be contacted is where the prescription was for a non-Part VIII product and the prescription hasn’t been endorsed with the invoice price, where required, for example if it is less common and there is no price held by the Pricing Authority. One way to reduce the volume of these returns would be for system suppliers to ensure that where there is no indicative price for the dispensed product on dm+d, there is a system control to ensure an invoice price is entered before the prescription can be sent for reimbursement. This is an area for pharmacies to discuss with their suppliers.
See also: Prescription returns.
Advance payment timescales: One month after the FP34C Form is submitted; pharmacy contractors receive an advance payment for prescriptions sent to the Pricing Authority with a deduction for prescription charges collected. One month later, once the prescriptions have been priced, pharmacy contractors receive the actual reimbursement for the prescriptions in question and the advance is recovered. See more on timing here.
Timescale for paper versus electronic: There is no change to this payment timescale with EPS R2. Community Pharmacy England continues to hold the view that the Government should pay community pharmacies more quickly and hopes that in the long term, the efficiencies offered by the EPS to the Pricing Authority will translate into quicker payments for pharmacy contractors.
Prescribing and pharmacy systems send and receive EPS messages via the central NHS Spine. Prescription information is linked with a patient’s NHS Number and medicines, but also various unique identifiers link the prescription with electronic dispensing and endorsement messages. These messages are received by the NHSBSA for reimbursement processes.
From time to time you may also look-up an old EPS prescription on your PMR system. This may be done so you can check pricing has been done correctly, or because the Pricing Authority have requested further information to price it.
A search may be carried out either:
- by patient or their NHS number where this is known;
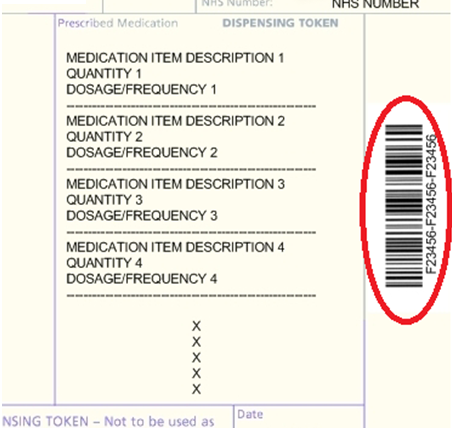
- using the EPS token ID or equivalent ID within barcode – ID (2) within the table; or
- using the UUID used within the Pricing Authority’s Transparency Portal if your system supplier allows yet – ID (7) within the table.
Eight key prescription identifiers (IDs) are listed below:
| Identifier category | Identifier | Information |
|
GP system-generated
|
(1) Prescription Form UUID* (long) | This universally unique identifier (UUID) is generated by the prescriber system. |
| (2) Short Prescription Form ID – token ID |
|
|
| (3) Prescription Line Item UUID* | Each line also has its own UUID. | |
|
Pharmacy system-generated: Dispensing
Note: If a dispense line or form |
(4) Dispense Notification Supplied Line Item UUID* | This line ID is generated for each dispensing episode entered onto the PMR system (e.g. owings). The Pricing Authority only need to receive last one. |
| (5) Dispensed Notification Form UUID* | Generated when pharmacy team sends the overall dispense message for form. | |
|
Pharmacy system-generated: Claiming
|
(6) Dispense/Claim Form UUID* | Generated when pharmacy team sends the overall prescription claim notification. Where claim amend feature used this will be regenerated. |
| (7) Dispense/Claim Supplied Line Item UUID* | This ID is used within the Pricing Authority’s Transparency Portal**. Speak to your system supplier about whether they will soon allow search by the Transparency Portal EPS ID if they do not already. | |
|
Generated for use by Pricing Authority
|
(8) Dispense Reimbursement Claim ID |
Spine generates this for sending to BSA, after pharmacy send final claim notification. Suppliers could not allow any lookup by this ID even if they wished to. This ID is only used by the Pricing Authority. |
*Indicates a ID composed of 32 characters plus four hyphens
**Information from the Pricing Authority. See column BP, of your Prescription Item report visible from within the Transparency Portal.
It is recommended that unique prescription identifiers should be treated like personal data. Although many people will not have the tools or datasets to be able to use the identifiers, the introduction of GDPR encouraged organisations to treat data sensitively even if only other individuals or organisations had the datasets which could reveal more behind the identifier.
Additional information:
- EPS identifiers – key information and info about identifiers within EPS HL7 messages.
- EPS developers library (developer.nhs.uk)
- EPS Tracker Application programming interface (API) – An EPS Tracker Application programming interface (API) exists so pharmacy system and software suppliers might build a bulk query interface in the future if wished.
See also: Using EPS identifiers webpage.
Endorsing EPS
Q. How will additional endorsements such as ‘XP’ be handled in EPS Release 2?
A. Information on the dispensed product, where required, will be provided to the Pricing Authority using the NHS dm+d SNOMED code for the product.
Other endorsements will also be required, in the same way as now, for example endorsements to claim broken bulk or out of pocket expenses or the NCSO concession. Pharmacy systems will support pharmacy staff in making these endorsements electronically. The guidance that has gone to system suppliers is in line with existing endorsement guidance.
Some pharmacy contractors currently make endorsements manually by hand without any support from their pharmacy systems. In these cases, pharmacy staff will in future be required to use their pharmacy system to make endorsements electronically.
Q. Can I endorse a prescription ‘NCSO’ in advance of the NCSO Concession being agreed by the Department of Health?
A. Yes, where a Part VIII product cannot be obtained at the Drug Tariff price because of a supply problem and a more expensive product has had to be dispensed, the prescription could be endorsed in anticipation of the NCSO Concession being granted. The full endorsement required is the initials, ‘NCSO’, full details of the product dispensed and the endorsement must be initialled and dated.
The Pricing Authority will reimburse based on the standard Part VIII price where the product was not been granted the NCSO Concession in the month concerned. The Concession is only granted where there is a significant national shortage. Detailed guidance on the NCSO Concession can be found in the stock shortages section of the Community Pharmacy England Website.
Q. How do we express that an EPS item is not dispensed?
A. Functionality varies from system to system, if you are unsure of how to mark an item as ‘Not Dispensed’ you are advised to check an up-to-date version of your system manual or contact your system suppler. The Pricing Authority endorsement manual (2013 version) mentions that “Prescribed items for which no dispensing activity has been recorded have the default item status code ‘0002’. When recording endorsements electronically within the Electronic Prescription Service the item status code ‘0002’ is used instead of an ‘ND’ endorsement.” The use of the letters ‘ND’ by pharmacy teams is for paper prescription endorsements only.
Submitting EPS
Q. Will the Pricing Authority (PA) allow me to amend a prescription after I have already sent it to them for pricing?
A paper prescription cannot be amended after the PA has received it for pricing.
However with electronic prescriptions, it may be possible to make a change (such as amending an incorrect endorsement or adjusting the patient exemption category) after the prescription claim message has been sent to the PA. This is subject to the following criteria:
- your PMR system supplier must have added the functionality required to recall claim messages,
- it must be before the deadline of the 5th day of the month following that in which supply was made.
After this time the PA’s pricing process will begin and the prescription can no longer be recalled.
If these criteria are met, your PMR system can allow you to recall, correct, and then resend the electronic script to PA.
Recheck processes may also apply within some scenarios.
Q. I have received a prescription and see that supplementary product information (e.g. ‘unlicensed’ or brand name) is included within the dose instructions area. Will the prescription be priced correctly and is this prescription valid?
There is the risk that the product information within the dose area will be missed by the patient/pharmacy and NHSBSA: With paper prescriptions it can easily be missed. With electronic prescriptions, standard pricing will be based on the product code of the prescribed product, therefore, supplementary product information included in the prescriber’s dosage instructions will not be considered when initially calculating payment. Some prescription may be re-issued by the prescriber onto paper and correctly. See further information in the EPS dispensing ‘Dosage area’ section and also at Avoiding EPS product info in dose area factsheet (Community Pharmacy England pdf one-pager) and cpe.org.uk/dosearea.
Q. Can I submit all of my electronic prescriptions at the same time?
Community Pharmacy England has received reports that submitting a large number of prescriptions at once can take considerable time depending on the system which is being used, and also whether there are any technical issues occuring on the local or national level at the time of the sending. Whilst sending prescriptions, you should ensure that Smartcard remains in place until all of the prescriptions which are being processed have been submitted.
Q. How can I reconcile the number of prescriptions I have submitted with the number which the Pricing Authority have priced?
Ensure that the total number of prescriptions submitted is included on the FP34C submission document, a copy can be taken for your records. Where the Pricing Authority identify a significant difference between your submitted total, and the number of prescriptions counted at the Pricing Authority, the pharmacy shall receive a phone call from the Pricing Authority. When the Schedule of Payments arrives, the number of items counted by the Pricing Authority should be similar to the number of items completed on the FP34C. For more assistance see here for further assistance on submission, and here for more information about claiming R2 scripts in time.
Q. I have part-dispensed an item and I’m waiting for the patient to collect the remainder. Can I claim for this item?
Pharmacist contractors would be expected to apply their judgement as to when and how much reimbursement to claim, as they do with paper prescriptions.
Q. The local prescriber frequently issues prescriptions for ‘Ensure Plus’ with the instruction ‘assorted flavours’, will this remain possible in EPS Release 2?
Yes, for food supplement/food replacement products, prescribers will continue to be able to request that a variety of flavours are dispensed. The GP’s prescribing system will support the prescriber in issuing a prescription using the products ‘Virtual Medicinal Product’ name and the prescriber endorsement to request that ‘Assorted flavours’ are dispensed. The pharmacy will continue to receive one Single Activity Fee for each flavour endorsed and dispensed, where assorted flavours are requested by the prescriber.
GP systems may have some remaining assorted flavour listings within their local databases for use with paper prescriptions, but EPS prescriptions can only be issued for items listed in the NHS database. There are not specific listings for ‘assorted flavours’ listed within the NHS database because the GP endorsement is needed instead for EPS dispensing and reimbursement.
Q. I have had to dispense a prescription from 2 different packs to make up the requested quantity. In the past, I would just endorse this on the form (e.g. 14 tablets from the 28 pack and 14 tablets from the 56 pack) and this would be taken into consideration when calculating reimbursement. Can I make an electronic reimbursement claim in this way?
Yes, 2 different SNOMED codes can be added to a dispensed “event” so for example if 50 tablets of Drug A were prescribed and the pharmacist has dispensed this quantity from 2 different available packs then the message would state:
Prescribed – Drug A snomed code with quantity of 50
Dispensed – Drug A pack size 1 snomed code with quantity
Dispensed – Drug A pack size 2 snomed code with quantity
Q. I have received a prescription requesting “Levothyroxine Sodium 100mcg tablets (Actavis UK)”. Do I have to dispense the Actavis brand and what will I be reimbursed for?
Levothyroxine sodium 100mcg tablets are listed in Part VIII of the Drug Tariff. When a prescription requesting generic “levothyroxine 100 mg tablets” is received the pharmacist can dispense any brand and will be reimbursed according to the Drug Tariff price for the product.
However, where a prescription for a generic product specifies the name of a manufacturer or supplier, legally and ethically that manufacturer’s product must be dispensed, and the pharmacist would be reimbursed based on the manufacturer or suppliers list price rather than the Drug Tariff price. Out of pocket expenses in procuring the product may be claimed, where appropriate. Guidance on out of pocket expenses can be found here.
Community Pharmacy England has received a number of reports of GPs inadvertently issuing prescriptions in this way because of the way products are listed in the picking-list of their prescribing system. This practice is not in the interests of patients, the NHS or community pharmacies. For example, this could lead to increased prescribing costs and delays in patients obtaining their medicine.
If contractors identify this as an issue in a locality, this is something that should be discussed with the prescriber.
Q. Do NHS Prescription Services begin pricing electronic prescriptions as soon as they are received in-month?
No. NHS Prescription Services only begin pricing electronic prescriptions once they have received the end-of-month submission form (FP34C). This form covers both paper and electronic prescriptions and is submitted together with the paper prescriptions dispensed in the month concerned.
EPS exemptions
Q. I have recently upgraded to EPS Release 2, do I need to record a patient’s exemption status in the electronic prescription claim message returned to NHS Prescription Services?
Yes. In EPS Release 2, pharmacy staff must mark every electronic prescription to indicate whether a prescription charge was levied, and where relevant indicate the prescription charge exemption category and whether evidence of exemption was seen. Where the patient is not age exempt or has paid the prescription charge, the reverse of a prescription or dispensing token also needs to be completed and submitted to the Pricing Authority along with the monthly paper prescription submission.
The Pricing Authority base payment solely on information contained in the electronic prescription message, therefore it is essential that prescription charge exemption information is recorded accurately in the electronic message to ensure correct payment.
Q. I have a prescription for a patient who was 59 when their prescription was written, however the patient did not declare age exemption until they were 60 at the time they collected the medicine. Is the patient exempt from paying a prescription charge?
Yes, subject to the prescription still being within the period of validity. Entitlement to prescription exemption can be based on the timing of the patient declaration rather than being based on the date the prescription was written. In this case, the patient was over 60 when they declared age exemption.
For EPS prescriptions, systems may compare the date of birth with the date of the dispense notification to determine whether age exemption automatically will apply. If the declaration date takes place at a different time, systems can allow the pharmacy staff to adjust age exemption manually.
The printed age on a prescription token or dispensing token may show the age at the time of the printing. Age exemption should be determined by the point at which the patient declares exemption rather than their printed age.
The Pricing Authority may issue penalty charge notices to patients where they determine there may be an issue. They should use the EPS token to help determine eligibility.
Q. If a patient brings in an EPS R2 prescription token from their GP Practice, can this be used to capture the patient’s exemption declaration where required?
Yes. Where a prescription charge exemption declaration is required, this could be captured on either a prescription token (the token printed by the GP Practice) or a dispensing token (the token printed by the pharmacy).
Q. I am dispensing an electronic prescription for a patient receiving income support. The patient needs to complete the prescription charge exemption declaration but I cannot print a token as my printer has run out of toner. How can I collect the patient exemption declaration in the interim until I can source a new toner cartridge?
The pharmacy has a number of options:
- Pharmacy staff could handwrite the dispensing token and use this to capture the exemption declaration. It is important to ensure that as a minimum, the patient’s name and the prescription ID number are written on the form. There is no need to write the product information or prescriber details.
- Some pharmacies have chosen to print additional dispensing labels and use these to support completing the token when the token printer is not available. If this approach is adopted, labels must include the prescription ID number. Whilst it is acceptable to place labels on tokens, labels should not be stuck on prescriptions as this could damage the high speed scanners at NHS Prescription Services; unlike prescriptions, tokens are not scanned.
- Another option is for pharmacy staff to record the patient’s exemption details, for example get the patient to write a note in a bound book with the name, date, prescription ID and their exemption details and then once the pharmacy is in a position to print tokens again, pharmacy staff complete the reverse of the token as the patient’s agent. The pharmacist would need to be sure that the patient understands that he has authorised the pharmacist to sign as his ‘agent’. However, this option is not recommended by NHS Protect and Community Pharmacy England for a number of reasons. Primarily because the pharmacist is involved in the transaction, insofar as they benefit financially from the dispensing of the prescription, and to help avoid any potential discrepancies between the patient and the pharmacist regarding exemption status. It should be noted, any liabilities incurred by acting as an “agent” are in fact liabilities of the patient and not the pharmacist acting as the agent. Therefore all liabilities for penalties will always be that of the patient. Unfortunately, Community Pharmacy England has been informed of cases where pharmacists or their staff have erroneously signed prescriptions on behalf of patients, where the patient was not present in the pharmacy at the time of dispensing, and the patients have received letters from the Counter Fraud officials seeking repayment where the patient was in fact not entitled to exemption from charges. To avoid any confusion between the pharmacist and patient, the signing of the exemption claim is therefore not recommended, unless the pharmacist or his staff see the proof of entitlement to exemption.
Printer problems such as a broken printer or running out of toner can create significant operational problems within pharmacies. It is important that pharmacies consider this in business continuity planning to minimise the risk of this occurring.
Q. I have received an electronic prescription for 4 items but when I’ve gone to print a token, it has printed over two tokens. Do I need to get the patient to complete the exemption declaration on both tokens?
It is not essential. It is sufficient to ask the patient to complete one token in this scenario. When the volume of text in an electronic prescription is greater than can fit on one token, there is provision for the electronic prescription to be printed over two tokens, for example 3 items on one token and 1 item on a second token. Both tokens link to the same electronic message and contain the same barcode and prescription identifier number. The patient declaration on the token is used to support prescription charge exemption fraud checks – asking the patient to complete one rather than both tokens is sufficient for this purpose – but both tokens should be submitted to NHS Prescription Services.
NHS Prescription Services base payment solely on information provided by the pharmacy and contained in the electronic reimbursement claim message, therefore it is essential that prescription charge exemption information is recorded accurately in the electronic message to ensure correct payment.
Q. In EPS Release 2, will my system be able to tell if a particular prescription includes ‘no charge’ items, for example a paid prescription for different strengths of the same drug?
This is no different to now. The number of fees and charges payable is calculated by NHS Prescription Services – the same pricing processes will be used with paper prescriptions. Likewise, pharmacy system suppliers have flexibility, as now, in how they develop systems to support the process, for example to support the pharmacy for reconciliation purposes.
Q. I received an electronic prescription for a contraceptive. The prescription was incorrectly marked as ‘paid’ when the reimbursement claim was sent. Will a charge be deducted during prescription pricing?
Prescriptions for products listed in the ‘No Charge Contraceptives’ section of Part XVI of the Drug Tariff, prescriptions for contraceptive devices listed in Part IXA of the Drug Tariff, spermicidal gels, creams, films and aerosols are automatically exempt from the prescription charge. As with paper prescriptions, even if the claim is marked as ‘paid’, no charge will be deducted for these items.
Electronic prescriptions for other drugs will also be exempt from the prescription charge if the prescriber has made the endorsement ‘CC’ in the prescriber endorsement field in the electronic message. Even if the prescription has been marked as ‘paid’ by the pharmacy, no charge will be deducted if the ‘CC’ endorsement has been made in the prescriber endorsement field.
There is no exception from the requirement to obtain a completed exemption declaration on the grounds that the patient has been prescribed a contraceptive.
Q. I have dispensed an electronic prescription for a special. Does the token with the patient’s exemption declaration need to go in a red separator?
No. Tokens are not used by NHS Prescription Services to price prescriptions, they are used for audit purposes (patient prescription charge exemption fraud) therefore there is no need to place tokens in the red separators. Tokens should be filed separately from prescriptions and do not need to be sorted in GP order.
EPS pricing accuracy
Q. How are EPS prescriptions priced?
When prescriptions are received electronically by the Pricing Authority they will be routed to a ‘rules engine’ which will support the automatic processing of prescriptions for pricing. It is hoped that this will improve the accuracy levels of prescription pricing as there will be less scope for human error which is a particular problem with current paper based processes.
Community Pharmacy England has a key role in conducting external audits of the accuracy of the Pricing Authority prescription pricing. Community Pharmacy England is in discussion with the Pricing Authority on the audits that will be conducted in future on the automated pricing of prescriptions submitted electronically. See also: Re-checks.
View the five minute video below to learn about the key EPS submission requirements:
Briefings and factsheets
- Comparing EPS total items: submitted vs priced
- EPS dose area: and exlcuding product info from within it
- Summary of EPS-related forms and tokens
If you have queries on this webpage or you require more information please contact it@cpe.org.uk. To share and hear views about digital developments with like-minded pharmacy team members, join the CP Digital email group today.
Return to the Pharmacy IT hub; EPS home or IT a-z index
For more information on this topic please email it@cpe.org.uk