Payment timetable and deadline tracker
Published on: 22nd February 2021 | Updated on: 19th May 2025
Community Pharmacy England has created a payment timetable and deadline tracker to assist pharmacy owners with checking and claiming payments for the following services:
-
- Appliance Use Review (AUR)
- Covid-19 Vaccinations (please note, this is a locally commissioned service)
- Discharge Medicines Service
- Flu Vaccination Service
- Hypertension Case-Finding Service
- Lateral Flow Device (LFD) Service
- New Medicine Service (NMS)
- Pharmacy Contraception Service (PCS)
- Pharmacy First Service
- Respiratory Syncytial Virus (RSV) and Pertussis Vaccination Service (please note, this is a locally commissioned service)
- Smoking Cessation Service (SCS)
- Stoma Appliance Customisation
The Pharmacy Quality Scheme (PQS) 2025/26 is also included in the payment timetable as well as details of other payments.
The table below outlines payments for services listed above, providing details of any claim deadlines (where applicable), how to claim, timing of payments, payment amounts and how these payments will appear on the Schedule of Payments.
| Payment type | Claim method (deadline to claim for payment) |
Payment due | Payment amount | How payment will appear on the Schedule of Payments under section of ‘Details of other amounts authorised’ |
| Pharmacy Quality Scheme 2025/26 declaration | MYS – Claims must be made between 9am on 2nd February 2026 and 11.59pm on 27th February 2026 | 1st April 2026 | The total funding for PQS 2025/26 is £30 million. The funding will be divided between qualifying pharmacies based on the number of points they have achieved up to a maximum £115 per point. Each point will have a minimum value of £57.50, based on all pharmacy owners achieving maximum points. Payments will be made to eligible pharmacy owners depending on the band they are placed in, how many domains they have declared they are meeting, and hence points claimed. | ‘Pharmacy Quality Scheme’ |
| Appliance Use Review (AUR) | MYS | Monthly |
£28 – AUR conducted on pharmacy premises £54 – AUR carried out in a patient’s home If, within a 24 hour period, reviews are conducted for several users living at the same location, the appliance or pharmacy owner may claim £54 for the first review and £28 for each subsequent review. |
Appliance use reviews carried out at premises Appliance use reviews carried out at patients home under section titled Prescription Fees |
| COVID-19 Vaccinations |
Must be recorded on the Point of Care system on the day of the administration of the vaccination. In exceptional circumstances, where it has not been possible to record the vaccination event, and the pharmacy owner has recorded the exceptional circumstances on the Point of Care, the vaccine record must be made on the system as soon as possible afterwards and within 15 days of the administration date of the vaccination. Where the record of the vaccination event is not created within 15 days of the vaccination being administered, the pharmacy owner shall not be eligible for the item of service fees and any associated additional payments Information will be transferred to MYS for claiming. Claims will only be accepted by the NHSBSA if they are submitted within three months of the date by which the claim should have been submitted. |
Monthly |
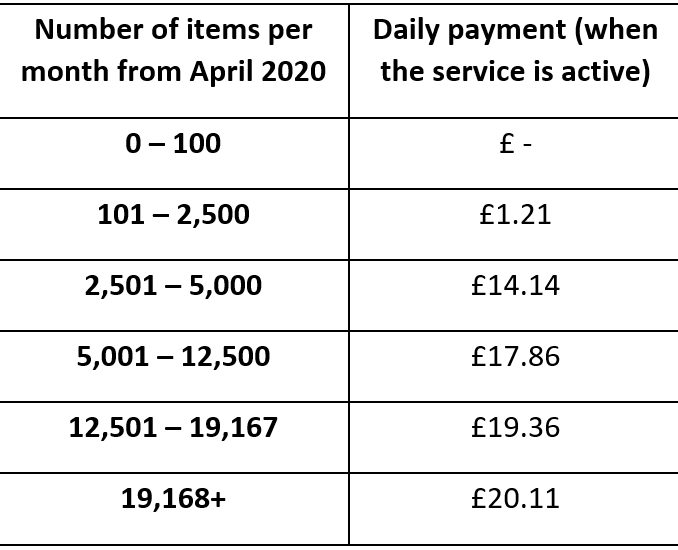
From 1st October to 31st March, £7.54 is paid for each dose of COVID-19 vaccination given to eligible patients . From 1st April to 17th June (spring campaign) and 18th June to 30th September (as part of the year-round offer), the payment for the administration of each dose of COVID-19 vaccination to eligible patients will be:
There is an additional financial supplement of £10 per dose for the vaccination of housebound people (cannot be claimed for vaccinations given in care homes). |
Covid Vaccine Claim |
| Discharge Medicines Service (DMS) |
MYS The claim for the stages of the DMS completed by the pharmacy owner must be made no later than the 5th day of the month following that in which the final stage that the pharmacy owner was able to undertake was completed. From 1 July 2024, if the contractor fails to submit by this deadline, later submissions will be accepted but only if made within three months of the date by which the claim should have been submitted. Later claims will not be paid. Where a pharmacy owner has completed some of the stages of the NHS DMS, but not all the stages of the NHS DMS that they intend to complete, they should not yet make a claim. . |
Monthly | 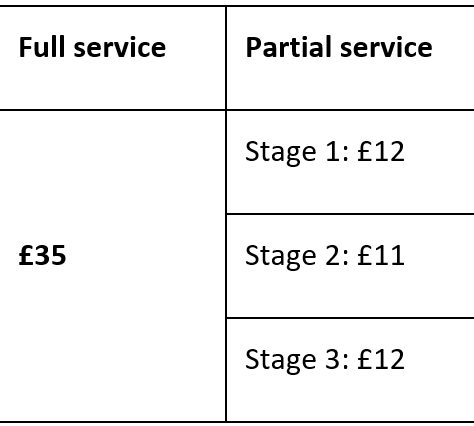 |
Discharge Medicine Review Fee |
| Flu Vaccination Service |
MYS Pharmacy owners must claim payment within one month of, and no later than three months from the claim period for the chargeable activity provided. Claims which relate to work completed more than three months after the claim period in question will not be paid and the pharmacy owner will not receive any payment for the administration of those vaccinations. |
Monthly |
£9.58 for each vaccine administered and The basic price (list price) of the individual vaccine administered and an allowance at the applicable VAT rate. |
Flu Remuneration Payment for fees Flu Reimbursement Payment for the cost of the vaccines |
| Hypertension Case-Finding Service |
MYS Claims for payment should be submitted within one month of, and no later than three months from the claim period for the chargeable activity provided. Claims which relate to work completed more than three months after the claim period in question, will not be paid. |
Monthly |
£440 set-up fee (one-off payment) From 1st April 2025, the fee for the clinic blood pressure check was adjusted from the previous fee of £15 to £10 per consultation. From 1st April 2025, the fee for ABPM provision increased from £45 to £50.85 |
CVD Hypertension set up fee CVD Hypertension check and ABPM fee |
| Late bundle – administrative charge | Claim form | Monthly | £25 | Late Fee |
| Lateral Flow Device (LFD) service |
MYS Claims for payment should be submitted within one month of, and no later than three months from the claim period for the chargeable activity provided. Claims which relate to work completed more than three months after the claim period in question, will not be paid. |
Monthly |
From 1st April 2025, the item of service (IoS) fee for the service has increased from £4.00 to £4.10 + VAT . An IoS will be paid for each completed transaction of the supply of one box of five COVID-19 LFD test kits and The payment for these tests, where supplied as part of the service, will be £6.80 for 5 LFD tests. An allowance at the applicable VAT rate will also be paid. The Secretary of State determines the payment of the LFD tests to be the average of the list price for one box of 5 LFD tests by the following three suppliers: AAH Pharmaceuticals Ltd, Alliance Healthcare (Distribution) Ltd and Phoenix Healthcare Distribution Ltd on or before the 8th of the month before. In circumstances, where pharmacy owners are unable to source one box of 5 LFD tests at or below the Drug Tariff payment price listed in this Part, Community Pharmacy England may request a review of the payment price. |
LFD Eligible Patient Service Fee
LFD Eligible Patient Test Cost |
| New Medicine Service (NMS) |
MYS Claims for payments for this service should be made monthly to the NHSBSA, in accordance with the usual Drug Tariff claims process. |
Monthly |
From 1st April 2025, the payment structure for NMS has been simplified to a £14 fee for each Intervention or Follow up consultation provided to the patient, i.e. a total fee of £28 will be paid if the pharmacy has undertaken both the Intervention and Follow up consultations. This change to the funding structure does not change the existing service requirement to undertake the Intervention consultation and to try to contact the patient to undertake the Follow up consultation. A £14 payment can only be claimed if a consultation has been undertaken with the patient. |
New medicine service under section titled Prescription Fees |
| Pharmacy Contraception Service |
MYS
Claims for payment should be submitted within one month of, and no later than three months of providing the chargeable activity. Claims which relate to work completed more than three months after the consultation will not be paid.
|
Monthly | A set-up fee of £900 per pharmacy, paid in instalments as follows:
£250 paid after claiming a further 5 consultations (i.e. 10 consultations completed) |
Contraception Set-Up |
|
From 1st April 2025, the consultation fee for both initiation and repeat supplies of contraception is £25 The cost of those medicines, if supplied as part of the service, will be reimbursed using the basic price specified in the Drug Tariff Part II Clause 8 – Basic Price. The total of basic prices will be added to the total basic price of products dispensed as part of essential services and the total will be subject to discount as per Part I Clause 5B paragraph 1. An allowance at the applicable VAT rate will also be paid. |
Contraception Consultations Contraception Product Cost |
|||
| Pharmacy First Service – consultation fee |
MYS
Claims for payment should be submitted to the NHSBSA by the 5th of the month following the month in which the chargeable activity was provided. If the pharmacy owner fails to submit by this deadline, later submissions will be accepted, but only if made within three months of the date by which the claim should have been submitted.
|
Monthly |
From 1st April 2025, the consultation fee for Minor illness consultations and Clinical Pathway consultations that passes the gateway point increased to £17 (from £15). The fee for Urgent supply consultations remains at £15. |
PF UMS & MI remuneration payment (both urgent medicines supply and low acuity/minor illness) Pharmacy First Consultations (PFCP) (clinical pathway consultations) |
| Where urgent medicines or appliances are supplied as part of an Urgent Medicine Supply referral, the cost of medicines or appliances supplied will be reimbursed using the basic price specified in Drug Tariff Part II Clause 8 (Basic Price). For clarity, no other elements of the Drug Tariff in relation to reimbursement of medicines or appliances apply to this service, including the payments for consumables and containers. | PF UMS & MI reimbursement payment | |||
| For Clinical Pathway consultations, only those medicines listed in the PGDs or Treatment Protocol will be eligible for payment. The following Parts of the Drug Tariff will apply: Part II Clauses 8, 10 and 13, Part IV and Part V (including where no discount deduction is applicable as set out in Part II). The reimbursement price will be based on the Part VIII generic price of a medicine linked to the Actual Medicinal Product Pack (AMPP)* code and the quantity submitted by contractors as part of the claiming process for the products supplied under the service. If the AMPP code submitted is associated with a Virtual Medicinal Product (VMP) of a Virtual Medicinal Product Pack (VMPP) listed in Part VIII or is a different pack size, the unit price of the listed pack size in Part VIII will be paid. If the AMPP code submitted is associated with a VMP of two or more VMPPs listed in Part VIII but is different to the pack sizes listed, the unit price of the listed pack size nearest to the quantity supplied will be paid. An allowance at the applicable VAT rate will be paid for products supplied under the Treatment Protocol.*Please refer to the Editorial Policy document on the dm+d website for the definitions of AMPP,VMP and VMPP. |
Discount on schedule section under: Generic (PFCP) Branded (PFCP) Appliances (PFCP) DND (PFCP) Subtotal (PFCP) Payment for consumables section: PFCP Payment for containers section: PFCP |
|||
| Pharmacy First Service – monthly fixed payment | Pharmacy owners do not need to claim this. NHSBSA will calculate whether a pharmacy owner is entitled to this payment, based on the number of clinical pathway consultations claimed that month. | Monthly |
£1,000 From 1st June 2025, a banded approach will be added to the monthly payment:
|
Pharmacy First Payments (PFCP) + Month |
|
RSV and Pertussis Vaccination Service |
To be confirmed.
|
Monthly | £9.58 for each vaccine administered |
Allocated local payment scheme code: 28: NHS RSV vaccination service; or 29: NHS pertussis vaccination service, as applicable. |
| Smoking Cessation Service (SCS) set-up |
MYS or using the form on the NHSBSA website
|
One-off payment | £1,000 | SCS Set-up |
| Smoking Cessation Service (SCS) |
MYS or by email using a downloadable form – further information is available on the NHSBSA website.
(Claims for payment should be submitted to the NHSBSA by the 5th of the month following the month in which the chargeable activity was provided. If the pharmacy owner fails to submit by this deadline, later submissions will be accepted, but only if made within three months of the date by which the claim should have been submitted).
|
Monthly | £30 – First consultation £10 – Each interim consultation £40 – Last consultation (the last consultation may be at any point from and including the 4-week review up until the 12-week review) |
SCS Consultations |
| The products that may be supplied as part of this service are listed in the Drug Tariff Determination and only those products listed will be eligible for payment. The indicative reimbursement price will be the NHS list price of the reference product on the 8th of the month before. An allowance at the applicable VAT rate will be paid to cover the VAT incurred when purchasing the product supplied. The indicative price for reimbursement for each product that can be supplied as part of this service is based on a reference product as set out in the list available on the NHSBSA website. | SCS NRT Product cost (this will include the VAT element) SCS NRT Product charges |
|||
| Stoma Appliance Customisation (SAC) |
Automatically based on qualifying Part IXC Drug Tariff products | Monthly | £4.32 is paid per qualifying* Part IXC item dispensed, regardless of whether customisation was required | Payment will be listed as Stoma customisation under section titled Prescription Fees |
Services where the claim deadline has expired
| Payment type | Payment due | Payment amount | How payment will appear on the Schedule of Payments under section of ‘Details of other amounts authorised’ |
| Pharmacy Quality Scheme 2025/26 Aspiration payment | 1st July 2025 | The maximum number of points for which a pharmacy owner can be paid an aspiration payment is 75% of the number of points available. The value of each point for the aspiration payment is set at £57.50 (i.e. the minimum value of a point for PQS 2025/26). | ‘Pharmacy Quality Scheme’ |
|
COVID-19 Vaccinations (1st April 2024 to 31 August 2024) |
Monthly |
£7.54 is paid for each vaccination given. From 1st April 2024 to 31 August 2024 an additional £2.50 (£10.04 in total) will be paid for each vaccination given. There is an additional financial supplement of £10 per dose for the vaccination of housebound people (cannot be claimed for vaccinations given in care homes). |
Covid Vaccine Claim |
| Hypertension Case-Finding Service – Incentive fees |
This incentive has now ended. Annually |
In addition, the following incentive fees across Years 3, 4 and 5 of the CPCF 5-year agreement, will be available. Pharmacies must reach a threshold of ABPM activity to trigger the payment of the incentive fee.
Pharmacy owners who sign up after Year 3 must achieve the ABPM activity thresholds specified for the given financial year and will receive £1,000 as a first payment. If a pharmacy owner signs up in Year 3 and fails to do 5 ABPMs, they can earn £1000 by doing 15 ABPMs in Year 4. Similarly, if a pharmacy owner first signs up in Year 4, they can earn £1000 by doing 15 ABPMs that year. If a pharmacy owner first signs up in Year 5, they can earn £1000 by doing 20 ABPMs that year. |
CVD Hypertension Incentive |
| Pharmacy Quality Scheme 2023/24 – Declarations could be made between 9am on 5th February 2024 and 11.59pm on 1st March 2024. | 2nd April 2024 | The funding will be divided between qualifying pharmacies based on the number of points they have achieved up to a maximum £137.50 per point. Each point will have a minimum value of £68.75, based on all pharmacy pharmacy owners achieving maximum points. Payments will be made to eligible pharmacy owners depending on the band they are placed in, how many domains they have declared they are meeting, and hence points claimed. | ‘Pharmacy Quality Scheme’ |
| Initial fixed payment for pharmacy owners who declared that they agreed to the terms and scope of the three elements of the Pharmacy First Service by 11.59pm on 30th January 2024 | 1st March 2024 | £2,000 | ‘Pharmacy First Initial Fixed Payment’ |
| Initial fixed payment for pharmacy owners who declared that they agreed to the terms and scope of the three elements of the Pharmacy First Service by 11.59pm on 31 December 2023 | 1st February 2024 | £2,000 | ‘Pharmacy First Initial Fixed Payment’ |
| Aspiration payment for the Pharmacy Quality Scheme 2023/24 | 1st November 2023 | The maximum number of points for which a pharmacy owner can be paid an Aspiration payment is 70% of the number of points within the band in which they are placed. The value of each point for the aspiration payment is set at £68.75 (i.e. the minimum value of a point for PQS 2023/24). | ‘Pharmacy Quality Scheme’ |
| Hepatitis C Testing Service | Monthly in the same payment month as other payments for NHS Pharmaceutical Services. This service was decommissioned on 31st March 2023 | £36 per test performed | ‘Hep C Provision of Testing Service’ |
| Hepatitis C Testing Service – Point of Care Test (POCT) kit | Monthly in the same payment month as other payments for NHS Pharmaceutical Services. This service was decommissioned on 31st March 2023 | Cost of the POCT kit at manufacturer’s list price + VAT | ‘Hep C Test Kit Reimbursement’ |
| Pharmacy Quality Scheme 2022/23 | 3rd April 2023 | The funding will be divided between qualifying pharmacies based on the number of points they have achieved up to a maximum £135 per point. Each point will have a minimum value of £67.50, based on all pharmacy owners achieving maximum points. Payments will be made to eligible pharmacy owners depending on the band they are placed in, how many domains they have declared they are meeting, and hence points claimed. | ‘Pharmacy Quality Scheme’ |
| Aspiration payment for the Pharmacy Quality Scheme 2022/23 | 1st December 2022 | The maximum number of points for which a pharmacy owner can be paid an Aspiration payment is 70% of the number of points within the band in which they are placed. The value of each point for the aspiration payment is set at £67.50 (i.e. the minimum value of a point for PQS 2022/23). | ‘Pharmacy Quality Scheme’ |
| Pharmacy Earlier Payment Scheme (PEPS) – transitional arrangements |
1st November 2021 – Bridging payment 1st December 2021 – recovery of bridging payment starts (this is spread over 11 months) |
1st November 2021 – One-off bridging payment based on 92% of the final PEPS payment received on 1st October 2021 1st December 2021 – 30th September 2022 – one-off bridging payment recovered in equal parts over 11 |
Bridging payment will be paid directly to PEPS pharmacy owners and will not appear on the Schedule of Payments Bridging payment recovery – ‘PEPS Transition Recovery’
|
|
COVID-19 Vaccinations (Care home incentive payments) |
This incentive has now ended. Claim via real-time return accessed via the QR or through Care Home Visits: COVID-19 Vaccinations Autumn 22/23 – Forms and Questionnaires (necsu.nhs.uk) Claims must be submitted within seven days following the visit (deadline for final claims 30th October 2022) |
5th September 2022 to 23rd October 2022 An incentive fee to support the vaccination of care homes residents based on home size was available and paid:£150 for each small care home (1-10 beds)£275 for each medium care home (11-49 beds)£400 for each large care home (50-149 beds)£525 for each very large care home (150-250 beds) |
‘Covid Vaccine claim’ |
| COVID-19 Lateral Flow Device Distribution Service |
This service has now ended. Claims will be accepted via MYS until 30th April 2022; this includes any distributions made in February 2022 that pharmacy owners may not have claimed for at the beginning of March 2022 |
From 4th October 2021 onwards £1.70 + an allowance for VAT per transaction – where a collect code has been provided OR £1.20 + an allowance for VAT per transaction using the anonymous collection route |
‘COVID Testing Kit’ |
|
Up until and including 3rd October 2021 £1.50 + an allowance for VAT per transaction |
|||
| Pandemic Delivery Service (Advanced service)* | The service ended on 31st March 2022. Pharmacy owners have until 5th April 2022 to claim payment | £6 (including VAT) per delivery | Payment will be listed as ‘Additional advance payment’ under section titled ‘Summary of Payment Amounts’ |
| Pandemic Delivery Service (Essential service)* | Monthly
Self-isolating patients only (from 1st April 2021 onwards) as confirmed by NHS Test and Trace (for the 10-day self-isolation period). This service will continue until 31st March 2022
|
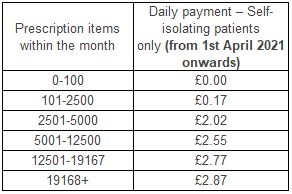 |
Paid on the same line as ‘Transitional Payment’. It will show as a total figure |
| COVID-19 Lateral Flow Device Distribution Service – Set-Up Fee | Before the service ended on 31st March 2022 | £250 + VAT | ‘COVID Test Kit Set up Fee’ |
| COVID-19 Vaccinations | Monthly |
£15.00 paid for each vaccination given between 1 December 2021 to 31 January 2022 £20.00 paid for each vaccination administered to patients during Sundays between 25 December to 3 January 2022 Additional £10.00 payment per vaccine for housebound and care home patients |
‘Covid Vaccine Claim’ |
| Pharmacy Quality Scheme 2021/22 | 1st April 2022 |
Maximum value of £135.50 per point Minimum value of £67.75 per point Points based system dependent on:
|
‘Pharmacy Quality Scheme’ |
| Pharmacy Quality Scheme 2021/22 – Aspiration payment |
1st December 2021 | 70% of the number of points within the band in which pharmacy owners are placed (the Aspiration Payment does not include the extra points that can be earned for being the Pharmacy PCN Lead). The value of each point for the aspiration payment is set at £67.75 (i.e. the minimum value of a point for PQS 2021/22). NHSBSA has published a spreadsheet detailing the banding that pharmacies have been put into for PQS 2021/22 |
‘Pharmacy Quality Scheme’ |
| COVID-19 Costs (incurred between 1 March 2020 – 31 March 2021 for the delivery of NHS pharmaceutical services) |
1st October 2021 |
Pharmacy owners could claim for the following: 1. Additional staff costs due to COVID-19 2. Costs incurred to make premises COVID-19 secure 3. IT and communication costs to support home working and virtual patient contact; and |
Reimbursement will appear as: ‘Reimbursement of Covid-19 costs’ Adjustment will appear as: Recovery will appear as: |
| CPCS –GP referral pathway engagement and set up | Payments depended on when the claim was submitted by a pharmacy owner and processed and verified by the NHSBSA | £300 engagement and setup payment if pharmacy owners undertook a range of actions to get ready for rolling out the referral pathway in their area by 30th June 2021 | ‘GP Referral Pathway Engagement Fee’ |
| COVID-19 Lateral Flow Device Distribution Service Early Sign-Up Fee | Registrations made from 29th March – 31st March 2021 were paid on 1st June 2021. Registrations made from 1st – 18th April 2021 were paid on 1st July 2021 | £200 + VAT Early sign-up fee (providing pharmacy owners signed up before 11:59pm on 18th April 2021) | COVID Test Kit Registration Fee |
| Pandemic Delivery Service (Essential service)* | Monthly – the service was extended until 31st March 2021 for all clinically extremely vulnerable (CEV) patients living in England | 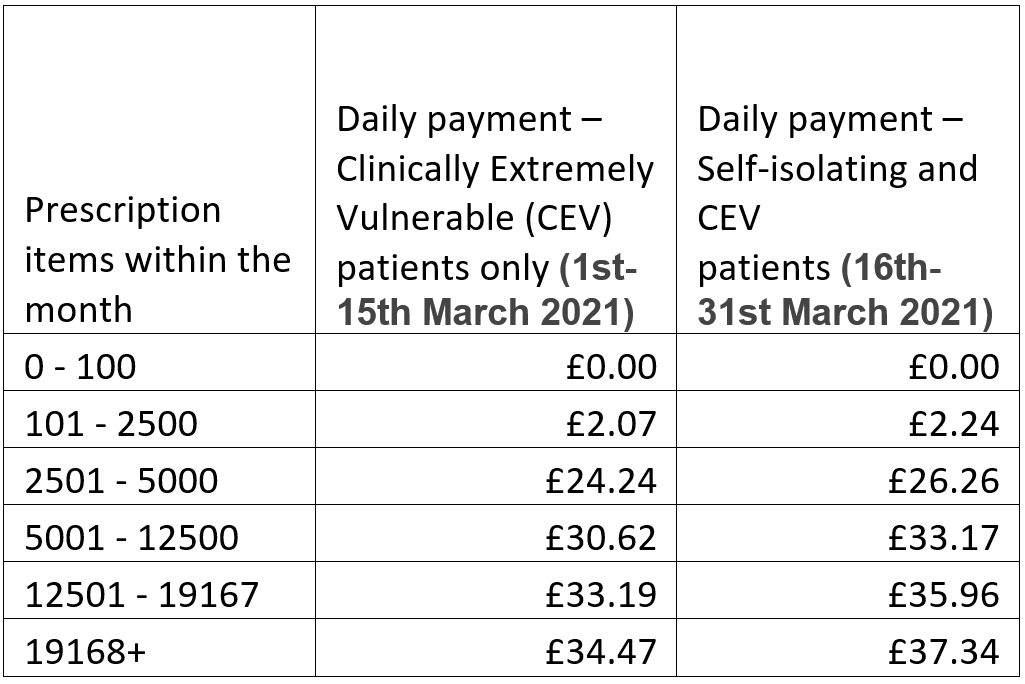 |
Paid on the same line as ‘Transitional Payment’. It will show as a total figure |
| Pandemic Delivery Service (Essential service)* | Monthly – service extended until 31st March for all clinically extremely vulnerable (CEV) patients living in England |
Payment bands up to end of February 2021 |
Paid on the same line as ‘Transitional Payment’. It will show as a total figure |
| Pharmacy Quality Scheme (PQS) 2020/21 Part 2 | 1st April 2021 | The funding was divided between qualifying pharmacies based on the number of points they have achieved up to a maximum £96 per point. Each point had a minimum value of £48, based on all pharmacy owners achieving maximum points | ‘Total of other amounts authorised’ |
| Discharge Medicines Service (DMS) set up fee | 1st April 2021 | Set-up fee of £400 covered the costs of preparing to provide the service, principally training staff and putting in place a standard operating procedure for the service. Any pharmacy on the pharmaceutical list on 1st February 2021 automatically received this payment | ‘Discharge Medicine Review Fee’ |
| PPE claims (standard) | PPE claims (standard) Payments depended on when the claim was submitted by a pharmacy owner and processed and verified by the NHSBSA. November 2020 Schedule of Payments which was paid on 1st February 2021 was the first available Schedule to include payments for PPE | 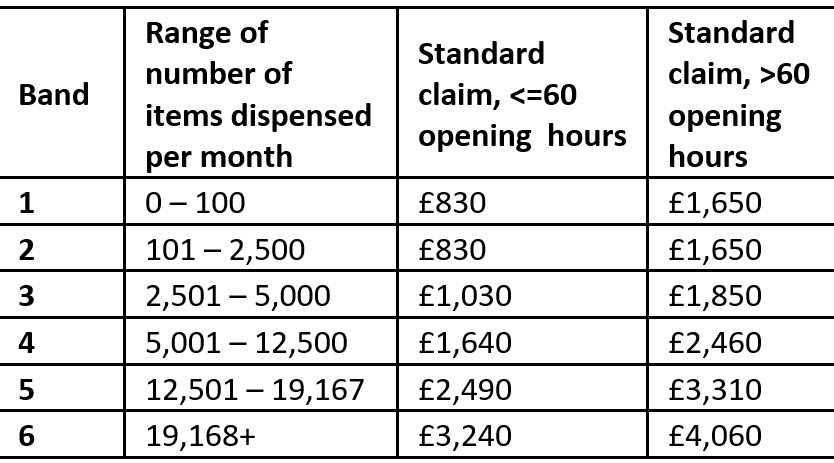 |
‘PPE Claims’ |
| PPE claims (exceptional) | As above | Depends on amounts claimed | ‘PPE Claims’ |
Further Resources
Factsheet: Using Your Schedule of Payments to Monitor Performance
For more information on this topic please email comms.team@cpe.org.uk