Submitting EPS and eRD messages within time
Published on: 12th August 2014 | Updated on: 11th November 2025
To help pharmacy teams avoid delays or loss of payment, this page explains how to manage timing for electronic prescriptions. Key information is also available in our Claiming for EPS and eRD prescriptions on time factsheet.
EPS prescriptions involve two key messages sent to the NHS Spine using your local IT system:
- Dispense notification (DN) – Sent during the dispensing process.
- Claim notification (CN) – Sent after the dispense message. This includes endorsement and charge status details. It may be called ‘electronic reimbursement claim’ or ‘prescription claim message’.
Examples of how pharmacy teams manage this:
- Checking before claiming: Some pharmacy owners may prefer that staff (e.g. locums) wait before sending the claim message, allowing time to check endorsements and exemption status.
- Tracking unclaimed prescriptions: IT systems may show a list of prescriptions nearing the 180-day EPS limit, helping staff submit claims before they go passed the 180 day limit.
Electronic Repeat Dispensing (eRD) prescriptions must be claimed within 365 days of the prescriber’s original signature date. Claims cannot be submitted after this deadline.
IT suppliers can add alerts and reports to help pharmacy teams avoid missing this deadline.
Discussion points for pharmacy owners and IT suppliers:
- What alerts will notify staff about eRD prescriptions nearing the 365-day limit?
- Will late eRD issues trigger extra warnings?
See the Tips section below for more on eRD timing.
To reduce the risk of payment delays—especially during unexpected closures—Community Pharmacy England recommends the following EPS submission tips:
EPS prescriptions:
- Send claim messages to NHSBSA by the 5th of the month after supply (Drug Tariff Part I, Clause 5A).
- Submit dispense and claim messages regularly (daily). Avoid waiting until month-end, as closures or technical issues could block submissions.
- Submit claim messages promptly for prescriptions with owings. For partial dispensing, mark the quantity (e.g. 14 of 28 tablets) and mark the rest as not dispensed.
- Follow the EPS 5-day window guidance (see below).
eRD and Controlled Drug (CD) prescriptions:
- Claim eRD issues within 365 days of the prescriber’s signature date.
- For Schedule 2, 3 and 4 CDs, dispensing must happen within 28 days of the appropriate date. Aim to send dispense and claim messages within this timeframe. IT systems may alert you, but won’t block submissions after day 28 in case dispensing occurred on time but messages were delayed (e.g. due to a technical issue).
Additional tips:
- Submit claim messages by the 5th of the following month (Drug Tariff Part I, Clause 5A).
- Submit messages frequently (ideally daily) to avoid delays and allow other pharmacies and NHS teams to check prescription status if needed.
- Mark all items correctly before claiming. If one item isn’t needed, mark it as ‘not dispensed’ so you can claim for the rest.
- Use the EPS 5-day window to ensure dispense messages are sent within the calendar month and claim messages by the 5th of the next month.
- Ensure Schedule 2, 3 and 4 CDs are marked as dispensed and claimed within 28 days.
- Claim eRD prescriptions within 365 days of the prescriber’s signature.
- Submit claim messages soon after the final dispense message and before the 180-day EPS deadline. After 180 days, NHSBSA cannot price the prescription.
IT system tips:
- Use filters to find prescriptions that still need dispense or claim messages.
- Learn how your system alerts you about prescriptions nearing the 180-day EPS limit or those downloaded but not yet dispensed.
- Use the EPS Tracker to check submission status using a prescription ID or NHS number. Read more.
- Use the claim amend feature (if available) before the 5th deadline. Plan for system updates that may disrupt submissions.
IT suppliers can help by adding alerts and reports to flag unclaimed prescriptions.
Discussion points for pharmacy owners and IT suppliers:
- What alerts will notify staff about prescriptions that may go unclaimed?
- Will the system show warnings (e.g. “X prescriptions dispensed over 3 months ago but not yet claimed”)?
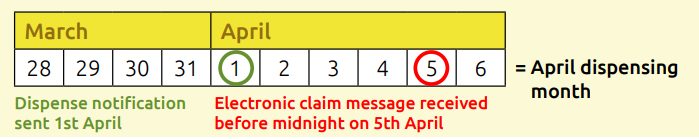
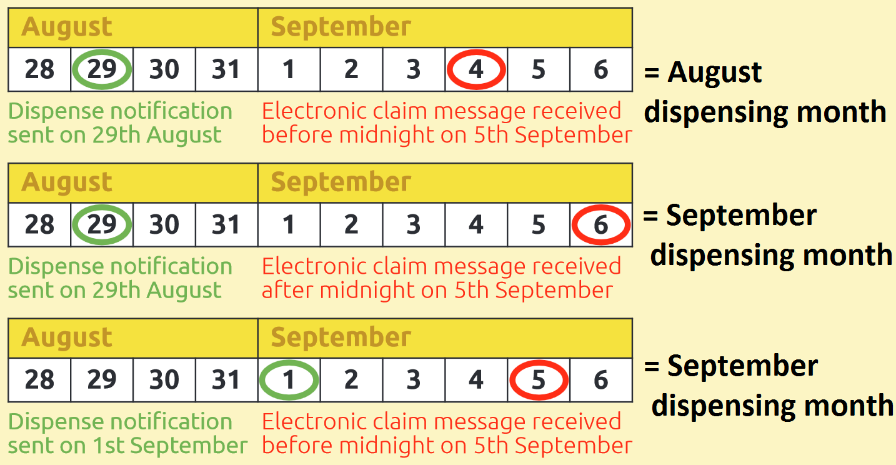
EPS prescription payments are based on two dates:
- Dispense message date
- Claim message date
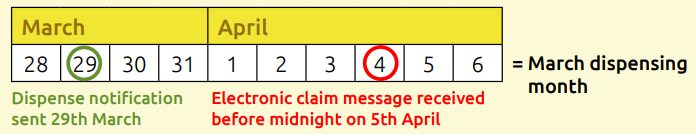
If the dispense message is sent before midnight on the last day of the calendar month, the claim message must be received by NHSBSA before midnight on the 5th of the following month to count for that dispensing month.
If the claim message is sent after the 5th, it won’t count for the original month.
Tip: Submit messages promptly. Prices for medicines and appliances can change monthly—e.g. if a price concession applies one month but not the next.
See examples below.
Following the explanation above, here are four scenarios showing how the timing of dispense and claim messages affects when your prescription is processed for payment.
Scenario 1: Both dispense and claim messages sent before the end of the dispensing month
Example: Dispense message sent on 29th March, claim message sent on 31st March.
→ This prescription will be processed as part of the March bundle.
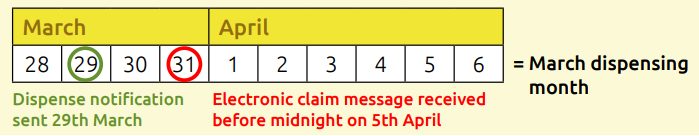
Scenario 2: Dispense message sent in dispensing month, claim message sent between days 1–5 of the following month
Example: Dispense message sent on 29th March, claim message sent on 4th April.
→ This prescription will still be processed as part of the March bundle.
Scenario 3: Dispense message sent in dispensing month, claim message sent after day 5 of the following month
Example: Dispense message sent in March, claim message sent on 6th April.
→ This prescription will be processed as part of the April bundle.
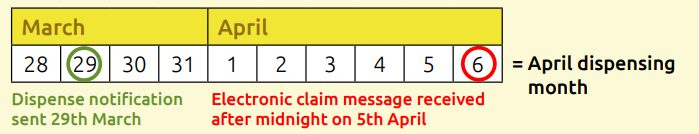
Scenario 4: Both dispense and claim messages sent between days 1–5 of the following month
Example: Both messages sent in early April.
→ This prescription will be processed as part of the April bundle.
Important:
In scenarios 3 and 4, the prescription will NOT be included in your March payment bundle—even if it was mistakenly declared in your FP34C submission for March.
What happens if EPS prescriptions go unclaimed?
Scenario A – Fully dispensed, no claim within 6 months
If a prescription is fully dispensed but no claim is submitted within 180 days, it will pass the deadline. It may still appear in your system, but NHSBSA will not process payment.
Scenario B – Partially dispensed, no claim within 6 months
If some items are dispensed but one item is left as ‘owing’ or partially dispensed, and no claim is made within 180 days, the prescription will pass the deadline.
→ Always claim for what was dispensed. Mark any undispensed items as ‘not dispensed’ and submit the claim.
Scenario C – No items dispensed within 6 months
If no items are dispensed within 180 days, the dispense message cannot be sent.
→ The patient should be referred back to the prescriber for a new prescription.
Scenario D – Patient needs further dispensing after 180-day deadline
If the patient needs more medication after the 180-day EPS limit, they must get a new prescription.
Prescriptions are held on the Spine for 3 months after the 180-day limit. No processing is allowed during this time. If a pharmacy tries to download the item, a rejection message will be sent.
Reimbursement after the 180-day deadline
Claims submitted after 180 days cannot be processed electronically.
→ In rare cases, a manual request may be made to NHS England, who may liaise with the NHSBSA—especially if the delay was outside the pharmacy owner’s control.
Claim messages must be submitted on time, and the correct number of items declared on your FP34C submission.
Your IT system can generate reports showing the number of EPS and paper items to include.
→ Do not count dispensing tokens—use the system-generated reports.
Comparing these totals can help identify prescriptions that haven’t been claimed in time.
Read more: Process for checking EPS total item numbers (reconciling) factsheet
In exceptional circumstances, where IT issues have prevented/delayed transmission of EPS claims to the NHSBSA, pharmacy owners are now able to submit a claim for these to be paid – as long as the claim is made within 12 months of the original deadline and suitable evidence of the IT issue is provided in support of the claim.
What counts as an IT issue?
Examples include:
- System supplier outages
- Software bugs
- Cybersecurity incidents
- Infrastructure failures
- Significant usability barriers linked to supplier-led changes
What pharmacy teams should do?
If you believe an IT issue has delayed or prevented EPS claim submission:
- Report the issue to NHSBSA as soon as it is identified.
- Raise it with your IT supplier or relevant NHS body promptly to support future validation.
- Keep records such as supplier confirmation, email chains, service desk tickets, and other verifiable documentation.
To be considered for payment:
- Submit the claim within 12 months of the original deadline.
- Provide evidence that the issue was outside your control and caused the delay.
- NHSBSA must be satisfied that the delay was directly linked to the IT issue.
This provision applies to claims for EPS prescriptions and has been reflected in the Drug Tariff (Part I, Clause 5A(4d)) since late 2025 (since 1st November 2025).
Q. I supplied a Serious Shortage Protocol (SSP) item within the SSP time period. Can I submit the SSP a bit late?
No. To avoid non-payment, SSP claims must be submitted both within the SSP timeframe and as part of the correct dispensing month bundle.
If you processed an SSP item on the last day of the calendar month—and that was also the final day of the SSP arrangement—you must ensure the claim is submitted on time.
For paper prescriptions, submit the SSP within the relevant dispensing month bundle.
For EPS prescriptions in this scenario, there are two options:
- EPS Option 1: EPS token SSP method
If there’s a risk of missing the deadline using the EPS SSP method, you can use the EPS token method instead. Submit the token with the correct EPS bundle to NHSBSA. - EPS Option 2: EPS SSP method
If using the EPS SSP method, consider the EPS 5-day window. If you couldn’t send the dispense message before the end of the month (e.g. due to a system outage), and the earliest you can submit is the next month, the SSP item will be late. In this case, use the EPS token method and submit it with the correct bundle.
Q. I have a prescription with both an SSP item and a non-SSP item. What if an owing delays submission and affects the SSP timing?
Pharmacy owners decide when to send EPS messages based on their systems and processes. However, if an owing delays submission, consider using the EPS token SSP method to ensure the SSP item is submitted on time. See the previous FAQ for more detail.
Q. I’ve dispensed two items on a prescription but only partially dispensed the third. How can I claim for the whole prescription?
If a prescription is at risk of reaching the 180-day EPS deadline, claim for the items that were dispensed. Mark any undispensed or partially dispensed items as “not dispensed” and submit the claim. Some pharmacy owners collect patient phone numbers to follow up on uncollected medicines.
Q. What happens if a price concession is announced after I’ve sent my claim message for an EPSR2 prescription?
Price concessions apply to the entire dispensing month. For example, a concession announced on 30th August applies to all prescriptions in your August bundle.
Your August bundle includes:
- Paper prescriptions sent to NHSBSA by 5th September
- EPS prescriptions submitted within the August dispensing month
Prescriptions are not priced until NHSBSA receives both the electronic and paper bundles, as the FP34C submission from the paper bundle is needed to calculate your advance payment.
How the dispensing month is determined for EPS prescriptions is explained below.
For more information on this topic please email it@cpe.org.uk