Pharmacy First service – FAQs
Published on: 5th January 2024 | Updated on: 29th May 2025
This page contains the answers to Frequently Asked Questions (FAQs) on the Pharmacy First service.
Return to the main Pharmacy First webpage
Click on a heading below for more information
Q. Who is eligible to provide the Pharmacy First service?
Any community pharmacy which meets the requirements for service provision can register to provide the Pharmacy First service.
Q. Is it compulsory to provide the Pharmacy First service?
No. As the Pharmacy First service is an Advanced Service in the Community Pharmacy Contractual Framework, pharmacy owners can choose whether they wish to provide this service.
Q. Is the Pharmacy First service a pilot?
No, the service is not a pilot; however, funding for the service is currently only guaranteed until the end of 2024/25.
Q. How does the national Pharmacy First service work?
The service involves providing consultations to give advice and NHS-funded treatment (via Patient Group Directions), where appropriate, for seven common conditions (clinical pathways consultations).
The consultations can be provided to patients who self-refer to the pharmacy (e.g. walk-ins) as well as those referred by NHS 111, GPs and others. The service also incorporated the previous Community Pharmacist Consultation Service (CPCS), meaning there are three elements to the Pharmacy First service:
- Pharmacy First (clinical pathways consultations) – new element
- Pharmacy First (urgent repeat medicine supply) – previously commissioned as the CPCS
- Pharmacy First (NHS referrals for minor illness) – previously commissioned as the CPCS
The seven clinical pathways cover sinusitis, sore throat, acute otitis media, infected insect bite, impetigo, shingles and uncomplicated urinary tract infections in women.
Q. Who helped to design the Pharmacy First service?
In designing the Pharmacy First service, NHS England worked with a team of experts to ensure that the service was developed with appropriate challenge, assurance, expert advice and consensus at every stage of the development process. This group included practising doctors, pharmacists, and specialists in areas like prescribing, children’s health, allergies, and antimicrobial resistance.
Alongside working with Community Pharmacy England, NHS England also sought input from representatives of organisations such as the National Institute for Health and Care Excellence, UK Health Security Agency and Royal College of General Practitioners. All decisions made by this group were consensus-driven and grounded in the latest evidence and national guidelines.
Q. What happened to the Community Pharmacist Consultation Service (CPCS)?
The CPCS ended on 30th January 2024 and the Pharmacy First service started on 31st January 2024, encompassing the minor illness and urgent repeat medicines elements of the CPCS.
Q. How do patients access the service?
Patients may be referred to Pharmacy First by one of the following organisations/routes:
- NHS 111 telephony or 111 online
- Integrated urgent care clinical assessment service (IUC CAS)
- 999 services
- General practice (low acuity minor illness conditions and the seven clinical pathways only)
- Other urgent and emergency care provider (e.g. UTC, ED, UCC)
Additionally, for the clinical pathway consultations only, patients can access the service by attending or contacting the pharmacy directly without the need for a referral.
Q. Do pharmacies need to provide all three services (i.e. Pharmacy First, Pharmacy Contraception and Hypertension Case-Finding) to receive the monthly payments?
DHSC and NHS England want to encourage pharmacy owners to provide all three services, but we pushed back on a proposal for compulsory provision of the Pharmacy Contraception and Hypertension Case-Finding Services for those wanting to provide the new Pharmacy First service. Instead, provision of all three services in a bundle is due to become a requirement to receive the monthly £1,000 Pharmacy First payment by 31st March 2025. Delaying the pace of this change will give pharmacy owners more time to prepare for and introduce the three services.
Q. What will happen to any locally commissioned Pharmacy First services?
Where locally commissioned services include one or more of the seven clinical pathways, we expect those elements of the local services will be decommissioned by the commissioner. We have worked with the affected LPCs to help them to identify other options which could potentially be discussed with the local commissioner.
Q. I am an LPS pharmacy owner; will I be able to provide the Pharmacy First service?
All the services to be provided by an LPS pharmacy owner must be agreed between the local service commissioner and the pharmacy and be included in their LPS contract. If LPS pharmacy owners want to provide the service, they should contact their local commissioner to propose a contract variation which includes the Pharmacy First service.
Q. My pharmacy doesn’t have a consultation room; can I provide the service?
No. Having a consultation room which meets the requirements in the Terms of Service is a prerequisite for the provision of the Pharmacy First service.
Q. My pharmacy has an exemption from NHS England on the requirement to have a consultation room. Can I, therefore, provide the service from a designated area in the pharmacy or outside my pharmacy?
No. It is a requirement of the service specification for pharmacies to have a consultation room which meets the requirements in the Terms of Service to provide the service.
Q. Is the Pharmacy First service only used out of hours, when general practices are closed?
No. Where appropriate for the patient, patients will be referred to a pharmacy during normal working hours. Consequently, the service must be available throughout the opening hours of the pharmacy (both core and supplementary hours).
Q. Can patients who do not live in England (for example, patients who live in Northern Ireland, Scotland or Wales, or tourists who are visiting England from abroad) access the Pharmacy First service?
Yes; such patients could be referred to the service by NHS 111, a GP or a UTC. Alternatively, when the person is in England, they could walk in/contact a pharmacy to access the clinical pathways strand of the service (subject to meeting the normal Gateway criteria).
However, remote consultations (telephone/audio or video consultations) for patients who do not live in England are not permitted, for example, a Scottish resident currently in Scotland cannot access the Pharmacy First service remotely from a pharmacy in England.
Q. Is a standard operating procedure (SOP) required for the Pharmacy First service?
Yes.
Q. Will NHS England cover the cost of procurement of an appropriate IT system to provide the service?
Procurement of an NHS-assured IT system to support provision of the service is the responsibility of the pharmacy owner.
Q. How do I inform NHS England that I intend to provide the Pharmacy First service?
Pharmacy owners must notify NHS England that they intend to provide the service by registering for the Pharmacy First service on the NHSBSA’s Manage Your Service (MYS) portal.
Q. Do I need to use MYS to state my intention to provide the Pharmacy First service for each pharmacy I own?
You can register each pharmacy separately via MYS, but multiple pharmacy owners can also use a bulk registration approach. Email the NHSBSA MYS team (nhsbsa.mys@nhs.net) to discuss how to bulk register pharmacies.
Q. Do I need to use MYS to register individual pharmacists to provide the service?
No. Pharmacies have to be registered, not pharmacists.
Q. Are there any requirements for the otoscopes used in the service?
Pharmacists conducting a consultation related to acute otitis media will need to examine the patient’s ears using an otoscope. Annex C in the service specification contains buying advice to guide pharmacy owners purchasing otoscopes.
Q. The service specification references the need for pharmacies (apart from Distance Selling Pharmacies) to have an otoscope. Do pharmacies need any other equipment?
The otoscope is the only equipment specified by the service specification, but pharmacy owners may want to consider having a thermometer which can be used to measure patients’ temperatures during consultation. Tongue depressors and a small torch may also help with examination of the throat, within the sore throat pathway.
Q. Do pharmacists have to do specific training programmes before providing the service?
No. Pharmacy owners must ensure that pharmacists and pharmacy staff providing the service are competent to do so, and are familiar with the clinical pathways, clinical protocol and PGDs. For some staff, this may involve completing some training programmes, but the learning needs of the individual will determine what training they need to undertake.
The Pharmacy First self-assessment framework, developed by CPPE and NHS England, can be used by pharmacists to consider their previous learning and experience in responding to minor illnesses in the pharmacy and to identify any gaps in their knowledge which they need to fill. Working through the self-assessment framework will also help them evidence to the pharmacy owner how they have achieved the necessary competence to provide the service.
Q. Do pharmacists have to undertake face-to-face training to provide the Pharmacy First service?
No, there is no requirement for face-to-face or any other specified training programmes which pharmacists must undertake before providing the service. The above FAQ provides more information on the competency requirements for the service.
Many pharmacists may want to undertake face-to-face training on ENT patient examination skills, including use of an otoscope, however this is not an absolute requirement for the service. .
Q. Is it compulsory to complete the CPPE/NHS England Pharmacy First self assessment framework?
No, use of the framework is not compulsory, but pharmacists will need a method by which to assess their competence and identify any gaps in their learning; the self-assessment framework is designed to help them do that.
Q. Do pharmacists need to complete a Declaration of Competence before providing the service?
There is no requirement to complete a Declaration of Competence, but pharmacy owners must ensure pharmacists are competent to provide the service. One way for pharmacists to demonstrate they have reviewed their own competencies is by working through the Pharmacy First self-assessment framework, developed by CPPE and NHS England.
Q. Do pharmacy owners need to update NHS Profile Manger when they start to provide the service?
No. When a pharmacy starts to provide the service, their Directory of Services (DoS) entries will be updated by DoS leads.
Q. Once a pharmacy is registered to provide the service, will it be visible in NHS Profile Manager?
No. As is currently the case for the Community Pharmacist Consultation Service, Pharmacy First will not be visible as a service provided by the pharmacy in NHS Profile Manager.
Q. Once a pharmacy is registered to provide the service, will it be visible in NHS Service Finder?
Yes. Pharmacy profiles in NHS Service Finder will show the pharmacy as being registered to provide the service.
Q. Once a pharmacy is registered to provide the service, will the service be listed on the pharmacy’s NHS website profile?
No. As was the case for the Community Pharmacist Consultation Service, Pharmacy First will not be visible as a service provided by the pharmacy on their NHS website profile.
Q. How often should I check NHSmail for referrals?
NHSmail may be used by some referring organisations, such as general practices. It is also used as the backup referral route, should the Pharmacy First IT system have an outage. If you do not ordinarily receive referrals via NHSmail, you could just check for referrals when a pharmacy opens and before the pharmacy closes each day. If you do regularly receive referrals via NHSmail, more frequent checking of the mailbox would be sensible throughout the working day.
Q. Do referrals into Pharmacy First need to be sent digitally or if the patient is verbally signposted can I treat this as a referral?
A referral within the NHS means one healthcare provider asks another healthcare provider to provide a service to a patient. As such, a referral requires a referral message to be sent from one provider to the other.
Where a patient is advised by one provider to seek assistance from another healthcare provider, whether that advice is provided verbally or in writing, that patient is being signposted to the other provider and not referred. Where a patient is signposted, the patient takes on the responsibility to make contact with the healthcare provider, as that organisation is not aware the patient has been directed to them.
Referrals to the Pharmacy First service need to be sent to the patient’s chosen pharmacy in a secure, electronic manner that complies with the standards laid out in the NHS CPCS Technical Toolkit; signposting does not count as a referral.
Q. How can healthcare professionals identify pharmacies providing the service, so they can refer patients to them?
Over 95% of pharmacies are signed up to provide the service and healthcare professionals can check pharmacy profiles in NHS Service Finder to identify which pharmacies are registered to provide the service. Additionally, if general practice teams use EMIS local or PharmRefer to make referrals to the service, participating pharmacies are shown in those systems.
Q. Is it still necessary for a general practice to send an electronic referral for the minor illness consultation part of the Pharmacy First service?
Yes, electronic referrals are still required for the minor illness part of Pharmacy First, as was the case for referrals to CPCS. They are also recommended for patients with symptoms suggestive of the seven clinical conditions covered by the clinical pathways.
Q. What are the benefits of general practices sending an electronic referral for minor illness consultations and clinical pathway consultations?
Submitting an electronic referral offers several benefits when compared to signposting. If referred:
- Patients will receive a confidential consultation with the pharmacist in the consultation room or remotely. If signposted, they may be assisted under the Essential support for self-care service, potentially being seen by another pharmacy team member.
- Patients may be more reassured that their concern has been taken seriously and the pharmacist will be expecting them.
- If the patient does not contact the pharmacy, the pharmacy will follow up with the patient, based upon clinical need.
- Referrals enable the pharmacy to plan and manage workload, helping them to see patients in a timely manner.
- Clinical responsibility for that episode of patient care passes to the pharmacy until it is completed or referred on.
- There is a record of referral and clinical treatment, which will support future patient care.
- Referral data can demonstrate that patients are actively being supported by their general practice to access appropriate treatment.
Q. How can general practices electronically refer patients to a pharmacy for a minor illness or clinical pathways consultation?
Referrals need to be sent to the patient’s chosen pharmacy in a secure, electronic manner that complies with the standards laid out in the NHS CPCS Technical Toolkit. There are several compliant ways in which referrals can be sent from within general practice IT systems, ‘bolt-on’ systems or NHSmail can be used. NHS England is currently in the process of developing guidance on the Pharmacy First service for general practices, but in the meantime, practices may want to refer to NHS England’s NHS community pharmacist consultation service toolkit for GP PCN staff. General practice staff could also contact their ICB’s community pharmacy clinical lead for further assistance on how this topic and in many cases, the Local Pharmaceutical Committee may also be able to provide advice to the practice.
Q. I am not receiving Pharmacy First referrals. How can I check whether I am listed on the Directory of Services as a provider of the service?
You can check whether your pharmacy is listed as a provider of the service in NHS Service Finder.
Q. A patient has contacted the pharmacy and said they had been referred for the Pharmacy First service, but there is no referral email or message in the Pharmacy First IT system. How do I proceed?
The pharmacist should check with the patient the name of the pharmacy that they were referred to and the referring organisation. If the patient has been referred to the correct pharmacy, the pharmacist should check again for a referral message. If no email or referral message is found, the pharmacist should contact the referring service, e.g. calling the NHS 111 Health Professionals Line (this number should be included in your SOP).
If the patient has been referred for assessment of one of the seven common conditions and passes the Gateway point in the relevant clinical pathway, they could be accepted as a walk-in patient.
Q. Can Pharmacy First consultations be provided remotely?
Where it is clinically appropriate to do so, minor illness consultations (referrals) and urgent medicines supply consultations (referrals) can be undertaken via telephone/audio or video consultation by a pharmacist who is on the pharmacy premises.
Similarly, where it is safe to do so, clinical pathways consultations can be conducted via good quality video consultation by a pharmacist who is on the pharmacy premises. Remote clinical pathways consultations can only be provided via a good quality video consultation – they cannot be provided by a telephone/audio consultation.
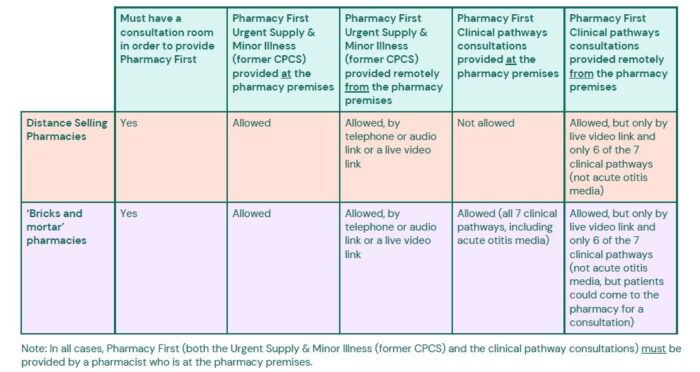
The various options for providing consultations are set out in the table below.
Q. Can remote Pharmacy First consultations be provided by a pharmacist who is not present on the pharmacy premises?
No. Any pharmacist providing the service must be at the pharmacy premises when providing a remote consultation to a patient.
Q. Can distance selling pharmacies offer the Pharmacy First service?
Yes, distance selling pharmacies (DSP) can offer the service, and where it is clinically appropriate to do so, minor illness consultations (referrals) and urgent medicines supply consultations (referrals) can be undertaken via telephone/audio or video consultation by a pharmacist who is at the pharmacy premises. Alternatively, those consultation types can also be conducted face-to-face with the patient at the pharmacy premises.
DSPs can only provide clinical pathways consultations via a good quality video consultation, conducted by a pharmacist who is at the pharmacy premises. They cannot provide this type of consultation with the patient being present at the pharmacy premises because the first part of any discussions with a patient relating to the clinical pathways consultations, prior to the Gateway point in the clinical pathway being passed, is part of the Support for the Self Care Essential service. DSPs cannot provide Essential services at their pharmacy premises.
DSPs are also limited to providing six of the seven clinical pathways consultations – the acute otitis media pathway is excluded as it requires otoscope examination of the patient’s ear.
Q. Why must pharmacies, including DSPs, carry out remote clinical pathways consultations by video consultation, rather than by phone?
This is because the conditions covered by the clinical pathways will often require the pharmacist to examine the patient (e.g. a rash) or examine a sample of urine, in the case of the UTI pathway. The service specification requires a live video link of sufficient quality to be used to carry out an examination, as part of the consultation.
The requirement to use video consultation only applies to clinical pathway consultations; pharmacies can continue to use the telephone for remote consultations for the urgent supply of medicines and minor illness consultations.
Q. Does the patient have to sign a consent form prior to the service being provided?
No. The patient needs to consent to receive the service and that should be recorded in the pharmacy’s clinical record for the service, but there is no need for the patient to sign a form to confirm consent – verbal consent is acceptable.
Q. Who can provide the service?
Only pharmacists can provide consultations as part of the service.
Q. Can trainee pharmacists provide this service?
Only a pharmacist can provide the service. However, with the consent of the patient, a trainee pharmacist could participate in the consultation to support their learning and development. For example, they could be involved in the discussion with the patient or examining them. A pharmacist would need to be present in the consultation to provide support and direct clinical supervision of the trainee pharmacist. That pharmacist would be responsible for the provision of the service and would retain professional responsibility for the care of the patient, including where necessary, making the decision on the supply of any medicine as an emergency supply or under one of the PGDs for the clinical pathways.
Q. Is there any advice available on which systems to use for video consultations with patients?
Our Virtual conferencing & remote consultations webpage provides advice and links to further information on this topic.
Q. Do NHS prescription charges apply where the patient receives a medicine as part of the service?
Yes. The normal prescription charge rules apply to medicines or appliances supplied under the service, whether via the urgent medicines supply part of the service or the seven clinical pathways. The Pharmacy First IT system will print off a prescription token and the patient should complete the relevant parts of the reverse of the form to claim exemption from the prescription charge or to indicate they have paid the NHS prescription charge.
Q. Can the prescription token for the patient to complete be printed on plain paper?
No. An FP10DT EPS dispensing token must be used so there is an exemption on the reverse which the patient can complete.
Q. What do I do with the prescription tokens patients have completed when a medicine was supplied as part of the service?
Where urgent medicines or appliances are supplied as part of an Urgent Medicine Supply referral the completed dispensing tokens should be sent to the NHSBSA as part of the month-end submission, clearly separated within the batch and marked ‘PF UMS’.
Where medicines are supplied as part of a Clinical Pathway consultation, the completed dispensing tokens should be sent to the NHSBSA as part of the month-end submission, clearly separated within the batch and marked ‘PF CP’.
Q. How do I find the NHS 111 Health Professionals Line telephone number?
NHS 111 providers have varying ways in which healthcare professionals can contact their teams. Check with your Local Pharmaceutical Committee to see if they can provide you with the local contact details for your NHS 111 provider(s).
Q. The patient’s name is not correct within the referring organisation’s referral. How do I proceed with making a record in the Pharmacy First IT system?
In this circumstance, you should be able to create a consultation record with the correct patient name by using the manual/back-up templates within the Pharmacy First IT system, making sure the referring organisation’s case ID is added to the new record.
Q. How does a pharmacy confirm the NHSmail address for a GP practice they do not usually communicate with?
Pharmacies can use NHS Service Finder to look-up non-public email and non-public telephone numbers (where available) for general practices. Pharmacies should then confirm with the practice that the identified email address is a suitable as a secure email that they can be used to send notifications or referrals to.
Q. Can I offer other NHS services, such as the Hypertension case-finding service to eligible patients when they visit for a Pharmacy First consultation?
Yes.
Q. If a pharmacy needs to temporarily close, what actions should be taken to manage Pharmacy First referrals?
In the event of a temporary closure, pharmacy owners must ensure the elements of their business continuity plan related to the service are activated and the service is temporarily withdrawn. They must inform the NHS 111 provider and local IUC CAS of the temporary withdrawal by calling the NHS Directory of Services Provider and Commissioner Helpline (0300 0200 363) as soon as possible to stop referrals being made to the pharmacy.
GP practices within your primary care network should also be contacted to prevent them making further direct referrals. The service commissioner (integrated care board) must also be informed by the pharmacy owner.
Q. How do I withdraw from provision of the service?
Pharmacy owners can withdraw from the service by providing one month’s notice and completing the Pharmacy First service withdrawn from service form via the MYS portal. Pharmacy owners may be asked for their reason for withdrawal from the service.
Q. Can patients see their Pharmacy First consultation records?
When GP Connect Update Record functionality is implemented, subject to the general practice making the record visible in online services, the Pharmacy First consultation record will be visible to the patient if they view their general practice record in online services such as the NHS app, NHS website account or GP patient apps.
Q. Where do I make my clinical record for the service?
Details and the outcome of each consultation must be recorded in the pharmacy’s Pharmacy First IT system.
Q. When should the clinical record be made?
Pharmacy owners must adhere to defined standards of record keeping, ensuring the consultation record is made on the same day that it occurs unless exceptional circumstances apply.
Pharmacists wanting to update their knowledge of best practice record keeping can access the CPPE Documenting in patient clinical records e-learning programme.
Making contemporaneous records at the time of the consultation is the expectation of pharmacists providing the service. This not only meets expected professional standards, but it also supports timely provision of data to the patient’s general practice, which will also become available to view by other pharmacists providing a consultation to the patient, should they need to seek further support in due course.
Q. What do I do if I cannot access my Pharmacy First IT system, e.g. due to an internet outage?
Where the Pharmacy First IT system is unavailable due to exceptional circumstances beyond the control of the pharmacy owner, then the consultation record must be added to the system as soon as possible after it becomes available again. If the problem persists for a period greater than 3 working days then the pharmacy owner must notify the local commissioner of the issue.
IT suppliers will make paper-based consultation record templates for pharmacists to use in business continuity scenarios, where the IT system is temporarily unavailable, e.g. due to a system outage or loss of internet connectivity.
Q. What happens during a Pharmacy First clinical pathways consultation?
In the confidential consultation, the pharmacist will ask the patient questions about their health. This may include their previous medical history, any allergies, any medicines they are taking and the symptoms they are currently experiencing. The pharmacist may ask the patient for consent to check any patient record they can access.
For some conditions, the pharmacist may ask to perform an examination, such as using an otoscope to examine the ear of patients presenting with acute otitis media symptoms. The pharmacist will be able to recommend the best course of action on an individual patient basis. A contemporaneous clinical consultation record will be made during the consultation and shared with the patient’s general practice to add to their clinical record.
Q. Are people not registered with a GP eligible for the service?
Yes. As well as providing the service, the pharmacy team could also explain how the patient can register with a GP practice. When entering the patient’s details on the Pharmacy First IT system, use the “unknown” option for their GP, to enable you to continue with the consultation.
Q. Can I supply OTC medicines as part of a clinical pathways consultation?
Bar the supply of Hydrogen Peroxide cream (which is an OTC medicine) under the treatment protocol for impetigo, no other OTC medicines can be supplied as part of clinical pathways consultations. Similarly, the supply of OTC medicines is not part of minor illness consultations. If a patient has a need for an OTC medicine, the NHS guidance expects them to purchase that themselves. If there is a locally commissioned minor ailment service and the patient is eligible to receive an OTC medicine under that service, that could provide an alternative option for the patient.
Q. Within the acute sore throat clinical pathway, do patients with a FeverPAIN score of 2 or 3 pass the Gateway point when they have a consultation with the pharmacist?
Yes. During the consultation, the pharmacist will be providing advice on self-care, including pain relief, and they will also be explaining to the patient that an antibiotic is not appropriate in their circumstance. They will also advise the patient to return if there is not improvement in 3-5 days. A clinical record for that consultation will be made to support any future consultations with the patient, and the consultation will pass the Gateway point, meaning a consultation fee will be paid.
Q. Will the Pharmacy First consultation fee be paid for consultations with self-presenting (walk-in) patients who do not pass a Gateway point in the relevant clinical pathway?
No. For self-presenting patients, a fee will only be paid where the consultation is provided and the patient’s condition/situation passes a Gateway point in the clinical pathway. The discussions with these patients will incur a cost for pharmacy owners, which is a concern for Community Pharmacy England and is one of the reasons we negotiated the £1000 monthly payment which will be paid to pharmacies providing the service, subject to them meeting the minimum clinical pathway consultation numbers set out in the Drug Tariff.
If a patient is referred to the service electronically (so the referral information is digitally transferred to the community pharmacy), e.g. by a general practice, if they do not pass a Gateway point in the clinical pathway, the patient can still have a consultation under the minor illness consultation part of the service and a consultation fee will be paid for that.
Q. Can a self-presenting (walk-in) patient who passes a Gateway point in one of the clinical pathways then receive a minor illness consultation?
No. Such patients can only receive a clinical pathways consultation, which subject to the individual pathway and relevant PGDs may or may not result in the provision of a medicine.
Q. What should I do if the medicine specified in the clinical pathway is not available at the time of the patient consultation?
NHS England is currently considering the alternative options which could be offered to patients, where one of the medicines specified in the clinical pathway is not available. Those considerations will incorporate the need to avoid unnecessary use of antimicrobials in the circumstances where the treatment included in the pathway is not an antimicrobial (e.g. steroid nasal sprays).
Prior to NHS England providing further guidance on managing situations where a medicine is not available, the patient could be referred to another local pharmacy if it is likely that stock will be available elsewhere. If there is a general lack of availability of the product, the patient would need to be referred to their general practice, to be assessed and an alternative product prescribed, where clinically appropriate.
Q. If I have to refer a patient to another pharmacy, as the medicine they need, based on eligibility criteria in the clinical pathway and PGD, is not available at my pharmacy, will I be paid a consultation fee?
No. Where a patient has to be referred to another pharmacy, a consultation fee will not be paid.
Q. I work at a distance selling pharmacy. If I have to refer a patient to another pharmacy, as the medicine they need, based on eligibility criteria in the clinical pathway and PGD, cannot be delivered to them until the following day, but they need the medicine today, will I be paid a consultation fee?
No. Where a patient has to be referred to another pharmacy, a consultation fee will not be paid.
Q. Are diagnostic tests, such as urine dipsticks or sore throat swabs, used as part of clinical pathways consultations?
No. Currently there is not enough evidence to support their use. NHS England consulted its expert group which advised on the development of the clinical pathways and came to this decision after a lengthy discussion, including a detailed consideration of national recommendations and current evidence.
For the urinary tract infection pathway, the national guidance from UK Health Security Agency currently does not recommend a dipstick test if the patient has two or three key urinary symptoms and no other excluding causes or warning signs.
For the sore throat pathway, NHS England accepted the NICE recommendation that rapid tests for streptococcus are not recommended for routine adoption as their effect on improving antimicrobial prescribing and stewardship, and on patient outcomes, as compared with clinical scoring tools alone (such as FeverPAIN), is likely to be limited.
NHS England’s position on point of care tests will be reviewed should national guidance be updated or should the tests improve in diagnostic precision and clinical utility.
Q. Can patients self-present to a pharmacy for a clinical pathways consultation?
Yes, but to be eligible for the consultation (and hence for the consultation fee to be paid) the patient’s condition must pass a Gateway point within the relevant clinical pathway.
Q. Where a walk-in patient’s condition does not pass the Gateway point in one of the seven clinical pathways, must a consultation record be made?
While not a service requirement to make an entry in the Pharmacy First IT system, pharmacists can choose to make a clinical record of advice provided under the Support for self care Essential service.
Q. If a patient is referred for a clinical pathways consultation by a general practice or other NHS organisation authorised to refer patients to the service, but the patient does not pass the Gateway point within the clinical pathway, what do I do?
In that circumstance, a referred patient can have a Pharmacy First minor illness consultation with the pharmacist, including the provision of self-care advice, for which a consultation fee will be paid.
Q. Are transgender and non-binary people eligible for the UTI clinical pathway?
Based on recommendations from the NICE Quality Standards, the UTI clinical pathway is for cisgender women, non-binary people registered female at birth and transgender men (with no structural alteration to their urethra), aged 16 to 64 with an uncomplicated UTI.
Cisgender men, non-binary people registered male at birth and transgender women (including those who have had structural alteration to their urethra) should be referred to their GPs for management as they are more likely to have a complicated UTI and are therefore excluded under the Patient Group Direction.
The Patient Group Directions will be amended in due course to clarify inclusion/exclusion criteria and to include a glossary of terms from the Stonewall Organisation.
Q. Do patients presenting for the UTI clinical pathway need to bring a urine sample with them to the consultation?
The clinical pathway suggests that, where practicable, there should be a visual inspection of a urine sample by the pharmacist to check if it is cloudy.
Where the pharmacy has contact with the patient prior to them presenting in the pharmacy, they could be asked if they could bring in a sample. If the patient does not or cannot bring a urine sample to a consultation in the pharmacy, the patient could be asked whether they have noticed any clouding of their urine.
Q. How should I dispose of otoscope and ear thermometer covers and tongue depressors following use in the examination of a patient?
Within the Health Technical Memorandum 07-01: Safe and sustainable management of healthcare waste such single use items are classified as offensive waste – see page 81 of the document (2022 version). This is not clinical waste, but may contain body fluids, secretions or excretions and it needs to be disposed of in yellow and black-striped ‘tiger’ bags.
Q. Can I dispose of offensive waste, such as otoscope covers and tongue depressors, in a clinical waste bin?
The Health Technical Memorandum 07-01: Safe and sustainable management of healthcare waste advises before disposing of an item in the infectious waste stream [clinical waste], consider whether the item is hazardous, or in fact just unpleasant. The over-classification of offensive waste as infectious waste can lead to more expensive waste management handling and treatment of such wastes. If there is no good reason to believe the item is hazardous – i.e. infectious, chemically / pharmaceutically / cytotoxically contaminated or radioactive – do not dispose of it to a yellow, orange or purple [clinical waste] bin/bag or other container for hazardous waste – see pages 81-82 of the document (2022 version).
Q. How do I dispose of offensive waste bags/containers?
Seek advice on this from your waste disposal contractor. The Health Technical Memorandum 07-01: Safe and sustainable management of healthcare waste provides guidance on waste disposal processes to be used by waste contractors (pages 82-93, 2022 version).
Q. How have concerns around antimicrobial stewardship been addressed in the design of the service?
NHS England has led work to ensure that the clinical pathways for the Pharmacy First service and the associated Patient Group Directions (PGDs) will allow community pharmacists to supply antimicrobials, only where clinically appropriate, without increasing the risks of antimicrobial resistance (AMR). A large number of experts have fed into this detailed programme of work, supported by clinical pharmacists from Specialist Pharmacy Service. The participating experts have included AMR Consultant Pharmacists, Infection Control Specialists (medical), the UKHSA’s ESPAUR team, senior GPs, academics, Primary Care Network clinical pharmacists, NHS England’s Medical Director and Chief Pharmaceutical Officer. The UK’s Chief Medical Officer has also been involved in decisions made on the approval of the clinical pathways and PGDs, alongside Government and NHS advisory committees on antimicrobial stewardship.
The clinical pathways for the service, set out requirements which the patient must meet (e.g. signs, symptoms and key diagnostic criteria, duration of illness, prior history of the same condition) to determine whether they may be suitable to receive a supply of an antimicrobial. The clinical pathways have been designed drawing upon the guidance provided to all primary care healthcare professionals in NICE’s Clinical Knowledge Summaries.
If those requirements are met, the requirements of the PGD will then be considered by the pharmacist, to assess whether it would be safe and appropriate to make a supply of the antimicrobial, or whether another option may be appropriate, such as delaying any treatment with an antimicrobial or referring the patient to their general practice, where clinically appropriate.
Pharmacists are highly trained healthcare professionals who understand medicines and their potential risks, and the experience of the Scottish and Welsh Pharmacy First schemes, not to mention many local services in England, suggests that pharmacists are more cautious about supplying antibiotics than other healthcare professionals. Pharmacists understand the issues and have already been contributing to anti-microbial resistance efforts for several years through their Pharmacy Quality Scheme.
Q. The UTI clinical pathway specifies ‘2 episodes in last 6 months, or 3 episodes in last 12 months’ as an exclusion criterion. Does this include the current episode that the patient is presenting with?
Yes, the current episode that the patient is presenting with would be included. Therefore, if the patient has had one other episode in the last 6 months and then presents with another episode, they would be excluded from the clinical pathway. If the patient has had two other episodes in the last 12 months and then presents with another episode, they would be excluded from the clinical pathway.
This same principle applies to other clinical pathways that reference a number of episodes within a defined period.
Q. A patient has returned to the pharmacy saying they have lost the medicine they were supplied with after their Pharmacy First consultation. Can I provide the patient with an additional supply of medicine?
As is the case with any medicine that is prescribed, there is no process to provide a replacement and claim additional reimbursement and remuneration if a patient has lost, spilled, or damaged their medicine. In the case when a medicine is prescribed, the patient would be required to obtain a new prescription before an additional supply could be made.
If a medicine was supplied as a result of a clinical pathway consultation but the patient is requesting a further supply of medicine, the pharmacist should confirm and verify (where possible) the circumstances as to why the patient no longer has their medicine (for example, was it spilled, lost, damaged). The pharmacist should document the details of the incident in the patient’s clinical record.
The pharmacist could then complete and record a new consultation and provide another supply of medicine, making a note on the clinical record of the previous loss of product and therefore supply of a new medicine.
In these exceptional circumstances, the pharmacist would need to complete and record a new consultation and new supply, making a note on the digital record of any loss of product, and submitting this new claim to the NHSBSA.
Q. Can I supply alternative medicines, forms or strengths to those listed in the PGDs or Protocol?
No. The medicines that may be supplied as part of the clinical pathway consultations element of this service are listed and detailed in each PGD or Protocol. Supplies of any alternative medicines, formulations or strengths are not permitted and will not be reimbursed.
Q. Do locum pharmacists need to sign the PGD authorisation sheet before providing the service?
Yes. All pharmacists, including locums, providing the Pharmacy First service and hence operating under the PGDs and protocol are required to sign the PGD authorisation sheet. That also needs to be authorised by an authorising manager, who may be the pharmacy owner or a manager employed by the pharmacy owner. A copy of this completed PGD authorisation sheet should be retained by the pharmacy owner as a record of those practitioners authorised to work under the PGDs and protocol.
Q. I am an independent prescriber. Can I prescribe under the Pharmacy First service rather than using the PGDs?
No. Any supplies of medicines made as part of clinical pathways consultations can only be made under the NHS England PGDs. In time, we hope that independent prescribers will be able to use their prescribing rights within this and other CPCF services, but the NHS England IP Pathfinder programme will first need to be completed.
Q. Can I supply more than one medicine to a patient who passes the Gateway point for the seven conditions e.g. for the acute sinusitis pathway, can I supply a nasal corticosteroid and phenoxymethylpenicllin at the same time?
No. Only one medicine should be supplied during a consultation (if the patients passes the Gateway point and it is clinically appropriate to do so). This applies to all the clinical pathways.
Q. If a patient presents with two or more different clinical pathway conditions, can I provide treatment for both and separately claim two consultation fees for the same patient?
Pharmacists should establish the priority consultation area, if it is felt that a patient has complex and multiple conditions, a decision would need to be made to determine if the consultation was suitable for Pharmacy First or in fact, needs to be escalated to a higher acuity setting.
Offering treatment under more than one clinical pathway could make it challenging to determine potential causes of side effects, allergies, and treatment failure.
Where you are not escalating the patient to a higher acuity setting and you are proceeding with treatment for a patient under one of the Pharmacy First clinical pathway conditions, you should agree with the patient the condition of most concern and provide support for that condition. Only one fee can be claimed for this consultation.
Q. I received a minor illness referral from NHS 111, but the patient needed an urgent medicine supply. Why did this happen and what should I do about it?
In some circumstances, where the patient is exhibiting symptoms, potentially due to not having taken their regular medicine, this may be referred as a minor illness referral, even though the patient’s eventual need is an urgent supply. This is the correct protocol, due to the patient being symptomatic and it can be managed by the pharmacist as an urgent supply referral; there is no need to ask the referring organisation to send another referral through. Your Pharmacy First IT system supplier will be able to advise you how to make an urgent supply record, when the referral has originally been sent through as a minor illness case; generally this will involve using the manual/back-up templates within the system, making sure the referring organisation case ID is added to the new record.
Q. Will the person at the referring organisation, for example, an NHS 111 health advisor assess the patient to determine if an emergency supply is appropriate under the Pharmacy First service?
No. The referring organisation should advise patients that the pharmacist may decide to make a supply of the medicine or appliance required, but the supply will only be made at the professional discretion of the individual pharmacist.
Q. Are staff at referring organisations, for example, NHS 111 health advisors required to include the name of the medicine the patient requires in the referral for an Urgent Supply under the Pharmacy First service?
No. Referrals may not contain details of medicines, as staff at the referring organisation may not be clinically trained, so they are not required to ask for that information. This means that staff will not identify if the request is for a Controlled Drug. The referral may come from the integrated urgent care clinical assessment service (IUC CAS) that is integrated with NHS 111 as a clinical call centre service using the same technical messaging as NHS 111.
Q. Can I reject an urgent supply Pharmacy First referral if it does not state what the patient is requesting?
No. Referrals may not contain medicine details, as many of the health advisors are not clinically trained, so they are not required to ask for that information. The pharmacist is required to conduct a private consultation with the patient to establish their needs before deciding how they can proceed with the service to best support the patient. The appropriate actions as a result of establishing the patient’s need, may include supply or onward referral if another action is required.
Q. Are patients who pay for their prescriptions eligible for a supply of an urgent medicine under the Pharmacy First service?
Yes. NHS prescription charges are collected as normal if an emergency supply is made as part of the service.
Q. I have received a Pharmacy First referral for an urgent supply while my pharmacy was closed. In what instances can such referrals be sent?
Pharmacy First referrals for urgent medicines supplies may be made to a pharmacy when the pharmacy is closed if the patient declares that their next dose is due within the next 2, 6, 12 or 24 hours. In such instances, the patient will be advised that they need to call the pharmacy when it is next open.
Q. Which medicines can I supply under the urgent supply strand of the Pharmacy First service?
Prescription only medicines (POMs) and prescription items that are not POMs that have previously been prescribed on an NHS prescription, can be supplied as part of the service where the pharmacist determines that it is appropriate to do so.
POMs must be supplied in line with the provisions of the Human Medicines Regulations. Prescription items that are not POMs can be supplied under this service if the criteria of the service are met (i.e. the supply is urgently needed, and it is an item previously provided on an NHS prescription to the patient). If a medicine or appliance which is not a POM is cheaper than a current NHS prescription charge and the patient is not exempt from prescription charges, the item can be purchased if the supply is within the product licence.
Claims to the NHSBSA for reimbursement for the cost of urgent medicines or appliances supplied will be made via the Pharmacy First IT system. The NHSBSA can only process these electronic claims; there is no paper claims process available for the service and electronic claims must use dm+d codes. It is possible that in some circumstances, a medicine or appliance may be requested that is not listed in dm+d, e.g. specials. Where it is deemed appropriate to make an emergency supply, but the item is not listed in dm+d, it will be necessary for the patient to be referred to another service which can issue an urgent prescription, such as the GP OOH service.
Q. How many days’ supply of treatment can I give a patient?
The pharmacist should apply their professional judgement to determine the most appropriate length of treatment to supply, in line with the provisions of the Human Medicines Regulations.
Q. Is there a maximum number of medicines or appliances that can be supplied as part of the service?
No. The pharmacist should apply their professional judgement to determine the appropriateness of making a supply of each requested medicine or appliance.
Q. Can I make an urgent medicine supply if a patient does not provide evidence of entitlement to exemption from NHS prescription charges?
Yes. Where a patient is unable to provide evidence of their exemption from NHS prescription charges, the pharmacy owner should record this on the FP10DT EPS dispensing token, in the usual way. NHS England may make checks on patients’ claims to the entitlement of exemption from NHS prescription charges.
Q. Do I have to follow local out-of-hours (OOH) prescribing guidelines?
Where local prescribing guidelines exist, they should be noted and act as a guide when considering whether it is appropriate to make an emergency supply.
Q. How does the urgent medicines supply aspect of the Pharmacy First service work in my area because there is already a locally commissioned emergency supply service in place?
In some areas, commissioners may decide to continue with a local walk-in scheme, and consequently, pharmacy owners may decide to provide both the local service and the Pharmacy First service. This is acceptable, but consideration would need to be given to how to avoid confusion between the two services and payment claims.
Q. Can I make an urgent supply of a Schedule 2 or 3 Controlled Drug for the treatment of epilepsy as part of the Pharmacy First service?
The legal requirements regarding the emergency supply of Controlled Drugs also apply to the Pharmacy First service. Emergency supplies of Schedule 2 or 3 CDs cannot be made, except for phenobarbital or phenobarbital sodium for the purpose of treating epilepsy.
Further advice on requests for controlled drugs
The urgent medicines supply strand of the Pharmacy First service follows the same rules and legislation as any other emergency supply.
A referral from NHS 111 does not automatically indicate that an emergency supply is appropriate; that is for the pharmacist to determine. Pharmacists who receive referrals for urgent supplies should use their professional judgement to determine whether an emergency supply is appropriate and legal to make. If it is not, the patient may need to be escalated to the GP OOH service or signposted to their own GP practice. Particular care should be taken when deciding to supply any medicine that has a potential for misuse.
The Human Medicines Regulations 2012 (HMR) set out the maximum quantity of a POM that can be supplied as an emergency supply. Professional judgement should be used to supply a reasonable quantity that is clinically appropriate, particularly where the requested medicine is liable to misuse.
To make sure urgent medicines supplies for Controlled Drugs are provided appropriately, please remember that:
- Emergency supplies of Schedule 2 and Schedule 3 Controlled Drugs are not permitted by the HMR, with the exception of phenobarbitone or phenobarbital sodium for the treatment of epilepsy;
- Temazepam, gabapentin, pregabalin and tramadol are all Schedule 3 Controlled Drugs. Emergency supplies of these medicines are not allowed and so they cannot be supplied via the service;
- Medicines such as benzodiazepines (apart from temazepam, which is Schedule 3), zopiclone, and zolpidem are Schedule 4 Controlled Drugs. Up to five days’ treatment may be supplied, if it is clinically appropriate and after an assessment has been made of the risk that the patient is using the service to inappropriately gain additional supplies;
- Medicines such as dihydrocodeine and codeine containing products (including co-codamol) are Schedule 5 Controlled Drugs. Up to five days’ treatment may be supplied if it is clinically appropriate and after an assessment has been made of the risk that the patient is using the service to inappropriately gain additional supplies.
- Where the legislation does permit an emergency supply, it limits the supply to a maximum of 5 days for Controlled Drugs;
- Some Integrated Care Boards have issued guidelines to local GP OOH services on the supply of medicines liable to misuse. Whilst it is for the pharmacist to determine whether a supply is appropriate, they should check if any such local guidelines are in place. The pharmacist needs to balance the potential for misuse versus the need and the impact on the patient of not supplying a medicine. A limited supply of up to 5 days treatment, until the GP practice reopens, may be appropriate. It is particularly important to check the patient’s National Care Record for such requests, as part of the assurance that the patient has been prescribed it before and that there has not been a recent supply made;
- A GP OOH service will only prescribe medicines liable to misuse in limited circumstances and will not usually prescribe medicines such as methadone or buprenorphine. If the pharmacist decides not to make a supply for a medicine liable to misuse, they should consider advising the patient to wait until they can collect their usual prescription from their GP practice or usual pharmacy, rather than referring them to the GP OOH service.
Q. I have received an urgent medicine supply referral for a patient; however, their GP practice is still open. What is the best way to proceed?
Patients should be advised to contact the GP practice if this is practically the most appropriate option to obtain their medicine or appliance. This may not be possible if, for example, the patient is away from home and unable to access their GP practice or where the GP practice will not be able to issue a prescription in a timely manner, such that the patient can get that prescription dispensed in time for their next required dose of the medicine. The pharmacist will need to assess each individual request and the circumstances of the patient to determine whether it is appropriate to make a supply via the Pharmacy First service.
Q. An urgent medicine supply referral has been sent for a patient requesting a Controlled Drug. Why has this occurred?
The majority of health advisors at referring organisations are not clinicians so do not assess the legality or clinical appropriateness of the emergency supply request. They are also not trained on the Human Medicines Regulations to determine what constitutes a valid emergency supply. A health advisor should advise patients when sending a referral that the pharmacy may decide to make a supply, however this will be at the professional discretion of the pharmacist.
If it is not possible to make an emergency supply due to prohibitions within the Human Medicines Regulations or other factors, but the pharmacist believes that there is a genuine patient need to obtain a supply of their medicine, the pharmacist must ensure the patient is able to speak to another appropriate healthcare professional by either:
- Referring the patient to their own general practice; or
- By contacting a local out of hours provider.
Q. What action should I take if an urgent medicine supply under the service is for a medicine liable to misuse?
While it is for the pharmacist to determine if a supply is appropriate, they should check if the Integrated Care Board has issued guidelines to local GP OOH services on the supply of medicines liable to misuse. This information should ideally be included in the pharmacy’s SOP for the service. The supplying pharmacist needs to balance the potential for misuse versus the need and the impact on the patient of not supplying a medicine or appliance. A limited supply of one or two days could be considered, to allow the patient time to access their GP surgery.
Q. If I don’t have an item in stock (Pharmacy 1) to provide an urgent medicines supply, how do I send the referral to another pharmacy (Pharmacy 2)?
Where it is appropriate for an emergency supply to be made, but the medicine or appliance is not in stock at the pharmacy (Pharmacy 1), with the agreement of the patient, the pharmacist will identify another pharmacy (Pharmacy 2) that provides the service, and which is convenient for the patient.
The pharmacist (Pharmacy 1) will contact the pharmacist at Pharmacy 2 to check whether they have the item in stock. If Pharmacy 2 confirms they have, then Pharmacy 1 will forward the electronic referral received from NHS 111 to Pharmacy 2 via NHSmail (the referral can be downloaded as a PDF) or the Pharmacy First IT system (if that functionality is available) and the pharmacist at Pharmacy 2 should contact the patient and follow the process in the service specification. In this instance, both pharmacies are eligible for the service completion fee.
Q. Can patients who do not live in England, such as temporary visitors or tourists, obtain an urgent supply of a medicine or appliance via Pharmacy First?
An urgent supply via the service is available to anyone in England who has recently been treated by the NHS and has received an NHS prescription for the item that is being requested. Patients treated in Wales, Scotland & Northern Ireland would be eligible, as would patients with prescriptions generated from other NHS organisations, for example, acute trusts.
For overseas patients visiting from countries outside the UK, an urgent supply under the service could be made for a patient who was receiving ongoing care under the NHS with an NHS prescription and needed an urgent supply of medicines to continue treatment. For example, this might include a patient who was recently discharged from an NHS hospital or who were treated on the NHS and had received an NHS prescription under a reciprocal healthcare arrangement.
Q. Can a patient use the service if they are not registered with a GP?
Yes. If a patient has been referred to the service for an urgent medicines supply and they are not registered with a GP, you may still make a supply if you decide it is legally and professionally appropriate to do so. This would include having checked the National Care Record Service to determine whether the patient has been prescribed the medicine or appliance recently and that the supply will meet the criteria set out in the Human Medicines Regulations. If the patient needs an urgent supply, but it is not appropriate to make such a supply, the patient should register with a general practice as a temporary patient for immediate and necessary treatment in order to obtain a prescription. You may also undertake a Pharmacy First minor illness referral and a clinical pathway consultation for a patient who is not registered with a GP. In all of these cases, it should be recommended to the patient that they register with a GP as soon as possible. When entering the patient’s details on the Pharmacy First IT system, use the “unknown” option for their GP, to enable you to continue with the consultation.
Q. Are housebound patients eligible for this service?
Yes. The pharmacist can interview the patient by telephone to make an assessment of the need for an emergency supply. However, if a patient who is housebound, needs an urgent medicines supply and is unable to visit the pharmacy, the pharmacist should use their professional judgement as to whether it is appropriate for a representative to collect the medication or appliance on the patient’s behalf.
Q. Are homeless people eligible for the service?
Yes.
Q. What can I do if my patient is unable to travel to the pharmacy to collect an urgent supply of a medicine?
If the patient is unable to travel to the pharmacy, the patient should be asked if there is someone they can ask to purchase or collect the medicine or appliance for them. Pharmacies are not expected to deliver medicines or appliances to patients as part of the service.
If this is not possible, the pharmacist will need to consider the impact of the missed dose(s). The pharmacist may want to suggest an appropriate alternative, for example referring the patient to a closer pharmacy offering the service or referring the patient to their GP. If requesting an urgent medicine supply, the patient could be referred to a local pharmacy not participating in the service to obtain an emergency supply of their medicine or appliance, but the patient would have to pay for any medicines or appliances supplied through this route.
Q. What should I do if a patient receives multiple referrals to the service over a short period of time?
Pharmacists are expected to use their professional judgement about any repeated requests for emergency supplies that are referred to their pharmacy. Any concerns should be raised with the patient’s GP as part of the feedback process, with a recommendation for a review. In some cases, it may be appropriate for the GP to add a Special Patient Note (SPN) to the patient’s care record to flag this issue to NHS 111.
Q. Can I refer patients to NHS 111 to access the urgent supply strand of the service?
Yes, in certain circumstances. If a patient requests an emergency supply from a pharmacy and the request meets the requirements of the Human Medicines Regulations and the pharmacist believes it is appropriate to make a supply, but the patient cannot pay for the emergency supply as a private service and it is also not practicable for them to obtain a prescription from their general practice before they next need a dose of the medicine, it may in those circumstances be appropriate to refer the patient to NHS 111. The patient should be advised to call NHS 111 so the call adviser can determine the most appropriate course of action for the patient, which may include offering them a referral to the service or potentially an appointment with the GP OOH service.
Q. Is the provision of an OTC medicine part of the minor illness consultation part of the service?
No. The outcome of referrals received in relation to low acuity conditions / minor illness may include giving self-care advice and support, the sale of OTC medicines, referral to locally commissioned pharmacy services, referral to the patient’s GP or relevant GP OOH service, or general signposting to other appropriate services (including other health professionals). Therefore, patients may have to purchase an OTC medicine if no locally commissioned minor ailments service exists.
Q. Can I refer the patient into another NHS pharmacy service?
Yes. Pharmacy services such as a local Minor Illness Service can be used where they are appropriate to meet a patient’s needs.
Q. I have received a minor illness referral while my pharmacy was closed. Is this a mistake?
Probably not, as the NHS Pathways system that guides the conversation between the referring organisation’s health adviser and the patient may identify that the best course of action is for the patient to speak to a primary care professional, such as a pharmacist, within a few days, rather than immediately.
Q. I have received a referral that says the patient needs to see a GP within 72 hours. Is this an incorrect referral?
Generally, no. The disposition names used in DoS and the NHS Pathways system can sometimes look like they are not appropriate referrals to community pharmacy, but despite some of the names/descriptors, they have all been clinically assessed as being appropriate for referral to and management in community pharmacy. Pharmacists should therefore deal with these Pharmacy First referrals as they would any others.
Q. What digital systems support the Pharmacy First service?
Pharmacy owners have access to Pharmacy First IT systems in which to make their clinical records for the service. These systems also automatically send data on service provisions to the NHSBSA’s MYS portal, via an application programming interface (API), which will populate the end of month payment claim.
The systems will also allow parts of the GP record to be seen, via GP Connect: Access Record (when this is made available) and they will send automatic updates to the GP record on the consultation and any medicines provided. This is a significant step forward towards the integration of pharmacy and GP care records that will support the future development of community pharmacy services. We have been pressing for this interoperability for many years, so the investment in it is very welcome.
Work is also being undertaken with NHS Pathways to develop their clinical triage system, to send electronic referrals from NHS 111 and Urgent and Emergency Care settings to community pharmacy that may otherwise go to a GP practice for the seven common conditions. Further work is ongoing with existing IT suppliers to streamline referrals from GPs to community pharmacies, moving those away from reliance on NHSmail.
Q. How do I raise an issue regarding Pharmacy First IT systems?
Pharmacy teams should contact the helpdesk of their Pharmacy First IT system to raise a ticket. Where the issue relates to one of the NHS-provided IT systems which is supporting the service, your Pharmacy First IT system supplier will escalate the issue to the relevant NHS IT team. This process is explained further in our Briefing on Reporting NHS IT, CPCF IT and EPS issues.
Q. Why are Pharmacy First Clinical Pathways consultations capped?
The overall budget for pharmacy services in England is limited and strictly controlled by DHSC, NHS England and HM Treasury (HMT). As part of the original introduction of the Pharmacy First service, there was a non-negotiable requirement from HMT that delivery of the service must be capped – they would not permit a ‘blank cheque’ for the service.
As pharmacy owners will know, despite the pharmacy sector receiving the largest uplift across the NHS in 2025/26, the pharmacy service in England remains significantly underfunded. As such, during discussions around the distribution of funding for 2025/26, both CPE and NHS/DHSC officials had to make very difficult decisions around the best way to deploy the limited funding available.
More of the limited funding available could have been allocated to fund more clinical pathways consultations in 2025/26, but this would have been at the expense of other funding streams, such as the increase to the Single Activity Fee. Ultimately, CPE and the Government’s agreed allocation means that the overall total volume of Pharmacy First clinical pathways consultations in 2025/26 can still grow substantially compared to the volume that was delivered in 2024/25. However, it is unlikely that the cap levels for the highest delivering pharmacies will reach the same heights that they did in 2024/25.
Note; caps are currently only in place for the Clinical Pathways element of Pharmacy First (i.e. the cap does not apply to Minor Illness or Urgent Medicine Supply). As part of the settlement for 2024/25 and 2025/26, it was agreed that CPE, DHSC and NHS England will together consider the potential for caps on other clinical services. This is in order to avoid ‘over commissioning’ by Government for services which they cannot afford to pay for under the limited Pharmacy budget, and thereby to avoid draining the contract sum which could impact other payments to pharmacies (such as dispensing fees).
This process may result in adjustment to caps for existing services or the implementation of new caps for services which are not currently capped; pharmacy owners would be notified of any changes in due course.
Q. Why are caps for Pharmacy First Clinical Pathways lower in April and May 2025 than they were at the end of 2024/25?
Caps on the number of consultations that can be delivered per month are based on actual delivery of Pharmacy First (clinical pathways). The mechanism for setting caps for Pharmacy First takes into account ‘underspend’, i.e. where caps are not met from earlier in the year, and it rolls this into allowances for later months. This mechanism meant that as the 2024/25 year progressed, more and more under delivered volume was rolled into caps, and these grew significantly.
However, as the under delivered volume for 2024/25 cannot roll into 2025/26 (HM Treasury rules do not allow transfer of unspent money from one financial year to the next), there is effectively a ‘reset’ of the system. The caps set from April 2025 are based on a target volume for 2025/26, but do not allow any under delivered allocations from 2024/25 to roll over.
As we progress through 2025/26, any under delivered volume will again be rolled over and used to increase allocations later in the year; depending on consultation numbers we may therefore again see the caps become higher later in the year.
Q. How do I find out what my cap is?
Details of cap levels for individual pharmacies are published by the NHSBSA on its website before the start of the applicable month.
The list published by NHSBSA indicates the band assignment and monthly cap for each pharmacy, by ODS code.
If a pharmacy’s ODS code is not included in the list, the pharmacy is automatically considered to be in Band 1 (the lowest band).
Q. How do I increase my cap?
A pharmacy’s placement within a band is based on their previous delivery of the service. For example, placements for May 2025 were based on pharmacy activity between Dec 2024 to Feb 2025.
Note; this means volume delivered in a specific month (e.g. Feb 2025) is taken into account for band placements 3 months later (May 2025).
The table below shows the activity required to be placed in the various bands for May 2025:
| Average monthly volume in Dec-24 to Feb-25 | Resultant May 2025 placement | May 2025 cap |
| Less than 16 | Band 1 | 32 |
| 16-21 | Band 2 | 42 |
| 22-25 | Band 3 | 53 |
| 26-30 | Band 4 | 62 |
| 31-37 | Band 5 | 75 |
| 38 or more | Band 6 | 132 |
For bands 1-5, the cap allowed in May 2025 is at least double the average volume delivered in the reference period – meaning these pharmacies would have potential to deliver more than they have historically done and then move up the placements in future months.
Band placements and cap levels will be updated monthly and published on the NHSBSA website.
Q. If a Pharmacy First clinical pathway consultation is provided over a pharmacy’s monthly cap, I won’t be paid a fee for the consultation, but will I be paid for any medicines supplied?
NHSBSA has confirmed that medicines will still be reimbursed for consultations which are over the cap.
Q. Do Distance Selling Premises (DSP) pharmacies need to be registered and able to deliver the Hypertension Case-Finding Service from 1st June 2025?
No. DSPs are exempt from the requirement of being registered and able to deliver the Hypertension Case-Finding Service. However, they will be required to be registered and able to deliver the Pharmacy Contraception Service, as well as Pharmacy First, and meet the minimum number of Clinical pathways consultations to be entitled to the monthly payment from 1st June 2025. This means the deadline for registering for the two services on the MYS portal is 11.59pm on 31st May 2025.
Q. Can a pharmacy choose to just provide Pharmacy First and not the Pharmacy Contraception Service and/or Hypertension Case-Finding Service?
Yes. The pharmacy can choose to just provide Pharmacy First and they will still be paid for the consultations they provide. However, they will not be entitled to the monthly payment even if they meet the minimum number of Clinical pathways consultations in a month.
Q. Will a pharmacy be automatically de-registered from Pharmacy First if they have not signed up to the Pharmacy Contraception Service and Hypertension Case-Finding Service* by 1st June 2025?
No. Pharmacies will not be automatically de-registered from Pharmacy First. As stated above, pharmacy owners can choose to just provide this service.
Q. If I’m not ready to provide all three services* by 1st June 2025, can I register for the services at a later date; will I then be eligible for the monthly payment?
Yes, you can register at a later date if you are not ready to register for the three services* by 11.59pm on 31st May 2025 and provide the services from 1st June 2025. If, for example, you are ready to provide the three services* by the middle of June 2025, if you then register on the MYS portal to provide all three* services by 11.59pm on 30th June 2025, you will be entitled to the July monthly payment if you also meet the minimum number of Clinical pathway consultations in July.
Q. If I have already registered my pharmacy for the three services* and have been delivering the services for a while, do I need to sign up again on the MYS portal to meet the bundling requirement?
No. If you are already registered for the three services* then you do not need to sign up again on the MYS portal to meet the bundling requirement.
Q. I am already registered on MYS for Pharmacy First and the Hypertension Case-Finding Service.* I have just registered on MYS for the Pharmacy Contraception Service; do I need to register again for Pharmacy First and the Hypertension Service* to show that I am now registered for all three services?*
No. If you are already registered for Pharmacy First and the Hypertension Case-Finding Service* you do not need to register again for these services.
Q. Will the bundling requirements for Pharmacy First change again in the future?
Yes, there will be further changes later in 2025/26:
- From October 2025, this requirement will increase to require pharmacy owners to deliver one ABPM consultation per month (this requirement does not apply to Distance Selling Premises (DSP) pharmacies); and
- From March 2026, this requirement will increase to pharmacy owners having to provide a specified number (on which Community Pharmacy England will be consulted) of Pharmacy Contraception Service consultations (including oral Emergency Contraception consultations), in addition to meeting the above requirements.
*Distance Selling Premises (DSP) pharmacies are exempt from the requirement of being registered and able to provide the Hypertension Case-Finding Service.
Q. How are pharmacies paid for providing the Pharmacy First service?
An initial fixed payment of £2,000 could be claimed via MYS from 1st December 2023 up to 23:59 on 30th January 2024. Pharmacies claiming this payment must provide 5 clinical pathway consultations by 31st March 2024 otherwise the payment will be recovered.
Pharmacy owners providing the service can claim the following:
- Service fee: £15 per consultation.
- Medicines reimbursement (where applicable): Where a medicine is supplied as part of this service, reimbursement will be paid, in line with the details set out in the Drug Tariff.
- Monthly fixed payment: £1,000 monthly can be claimed from February 2024 onwards, subject to meeting the clinical pathways consultation thresholds (see the table on our main Pharmacy First webpage).
Q. Is there a different consultation fee for referred patients compared to those that self-present to the pharmacy?
No, the same consultation fee (£15) is paid for all consultations.
Q. Will the consultation fee be paid for clinical pathway consultations which pass the Gateway point, but where a medicine is not supplied, as it is not clinically appropriate?
Yes, a consultation fee will be paid for consultations which pass the Gateway point, but where it is not clinically appropriate to supply an NHS medicine. In some cases where a medicine is not supplied, the clinical pathway may advise that the patient returns to consult a pharmacist after several days if the condition has not been resolved.
Q. Where a medicine is supplied under the service, is the reimbursement based on the electronic submission to MYS, from my Pharmacy First IT system, or the printed EPS token on which the patient declares their prescription charge exemption or payment?
Reimbursement is made on the electronic submission to MYS. The printed tokens completed by patients and submitted to the NHSBSA at month end are only used for the purpose of checking patients’ exemption claims.
Q. If I receive a referral but cannot contact the patient, can I claim the consultation fee?
No.
Q. Where a clinical pathway advises that the patient should return for a further consultation in certain circumstances (e.g. Sore throat FeverPAIN score 2 or 3) will another consultation fee be paid for the second consultation?
Yes.
Q. How are reimbursement prices determined for medicines supplied under the Pharmacy First service?
The reimbursement prices are based on the listed Part VIIIA Drug Tariff basic prices of generic medicines linked to the Actual Medicinal Product Pack (AMPP) codes and quantities submitted as part of the claiming process for this service.
The AMPP describes an actual product which is known to have been available linked to both the name of a particular supplier and information on the pack size of the product, for example ‘Mometasone 50micrograms/dose nasal spray (Sandoz Ltd) 140 dose.
Q. If I select and supply a particular brand of a medicine for example, ‘Mometasone 50micrograms/dose nasal spray (Sandoz Ltd) 140 dose’ will I be reimbursed as per the list price for this AMPP code?
No. The reimbursement is based on the listed Part VIIIA Drug Tariff basic price of the generic medicine associated with AMPP code submitted as part of the claiming process for the Pharmacy First service.
Q. Do the current discount deduction arrangements apply to medicines supplied under the Pharmacy First service?
Yes, the usual discount deduction arrangements apply, including the Discount Not Deducted (DND) status where no discount deduction applies if the medicine is listed in Part II of the Drug Tariff.
Q. Can I claim any out of pocket expenses or submit a broken bulk claim where applicable, for medicines supplied under the Pharmacy First service?
No. The IT developed for this service does not support claiming out of pocket expenses and/or broken bulk.
Q. Do price concessions apply to reimbursement of medicines supplied under the Pharmacy First service?
Yes, if a medicine is unavailable to purchase at or below the Basic Price listed in Part VIIIA of the Drug Tariff, the usual price concession arrangements will to apply to the reimbursement of any eligible medicine supplied under Pharmacy First service. Pharmacy owners should continue reporting any pricing issues using our reporting form.
Q. What VAT rate is applicable for supplies made as part of Clinical Pathways consultations?
In 2023, the Government announced that it would extend the zero rate on medicines prescribed on prescriptions to medicines supplied to patients under PGDs. HMRC subsequently announced that from 9th October 2023 to 31st March 2027, the VAT rate for supplies of medicines made to patients using a PGD would be set at the zero rate.
Therefore, a zero rate of VAT will apply to all medicines supplied using PGDs under the Pharmacy First service. However, an allowance at the applicable VAT rate will be paid for Hydrogen Peroxide 1% cream (Crystacide) as this is supplied under a Treatment Protocol (not a PGD).
Q. What VAT rate is applicable for urgent repeat medicines/appliances supplies made as part of the service?
The standard rate or reduced rate will apply to these supplies of products, as appropriate to the individual product supplied.
Q. Which budget will the cost of the medicines supplied under the service be charged to?
The cost of medicines supplied will be charged to the Integrated Care Board where the pharmacy providing the service is based.
Q. If we don’t agree with the Pharmacy First claim information pre-populated into MYS by our IT system, what should we do?
The claim information pre-populated into MYS comes from a direct feed from your Pharmacy First IT system, based on the consultation information you have entered into the system. If the data in MYS does not tally with your expectation, you should first check that all relevant referrals have been correctly processed in the IT system; if a consultation has not been completed within the system, it will not appear in your MYS claim. Any consultations subsequently completed after the month end will appear in the claim created for the subsequent month.
If the above guidance does not address the discrepancy, you should contact the IT system’s helpdesk.
For more information on this topic please email services.team@cpe.org.uk