CPCF settlement: 2024/25 and 2025/26
Published on: 7th April 2025 | Updated on: 7th January 2026
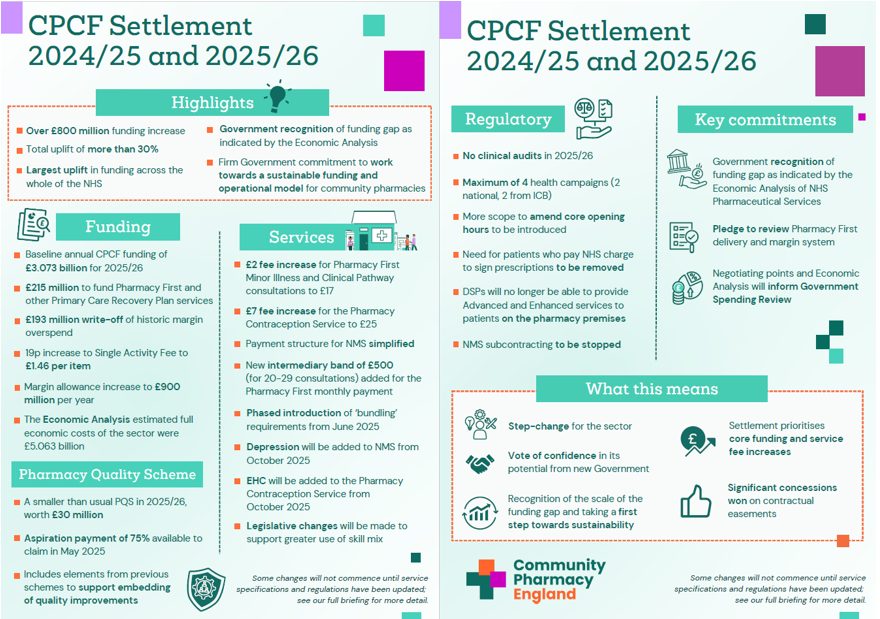
In March 2025, funding and other arrangements for community pharmacies for 2024/25 and 2025/26 were finalised. The settlement between Community Pharmacy England, the Department of Health and Social Care (DHSC), and NHS England provides community pharmacy with the largest uplift in funding across the whole of the NHS and signals the Government’s commitment to stabilising the sector, recognising the key role they will play in future healthcare.
Overview
The resources below set out information on the CPCF for 2024/25 and 2025/26 in a variety of formats to help pharmacy owners understand the key elements of the settlement.
In each section below we have outlined that element of the CPCF settlement in more detail.
The settlement takes baseline annual CPCF funding for 2025/26 to £3.073 billion and secures a further £215 million to fund the continuation of Pharmacy First and other Primary Care Recovery Plan services.
The level of allowed medicines margin for 2025/26 is being increased to £900 million, with £193 million of historic over-delivery also being written off.
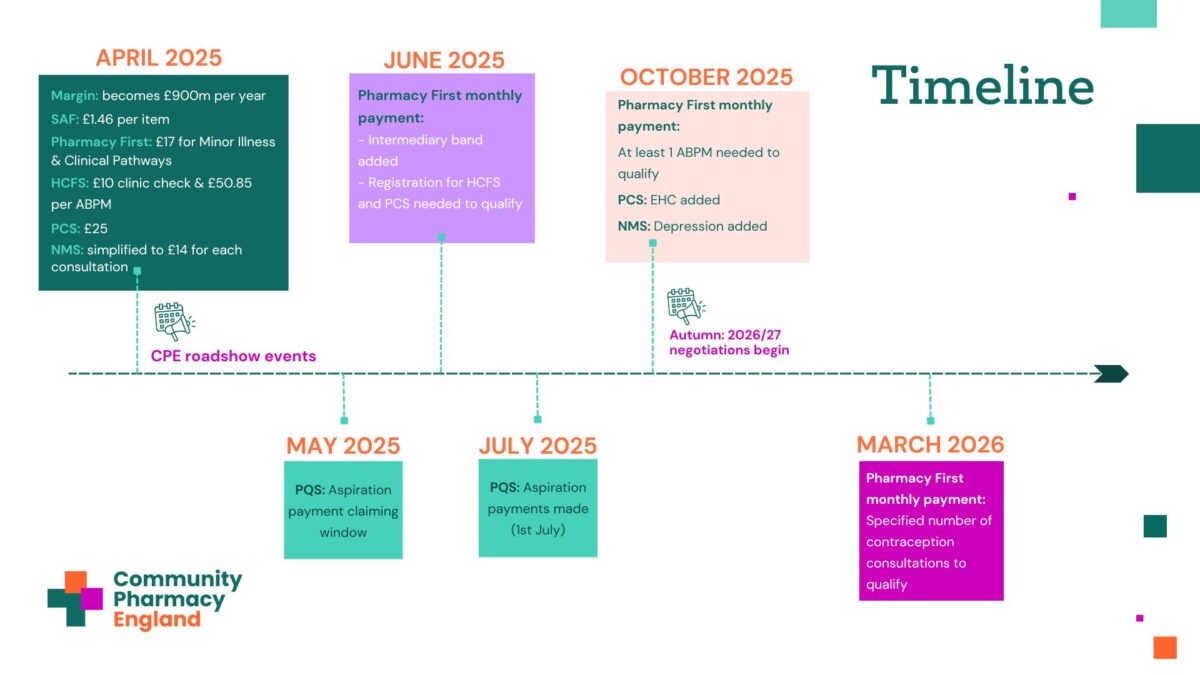
From 1st April 2025, the Single Activity Fee (SAF) increases to £1.46 per item.
April 2025 Drug Tariff updates
April 2025 Category M prices announced
Clinical services to be included in advance payments
Pharmacy First
Fees for the Minor Illness and Clinical Pathway consultations part of Pharmacy First are uplifted to £17, whilst the Urgent Medicine Supply fee remains at £15.
From June 2025, a banded approach will be introduced for the Pharmacy First monthly payment: £500 for those delivering 20-29 consultations per month and £1,000 for those that achieve 30 or more.
A phased introduction of ‘bundling’ requirements is underway. To receive the monthly Pharmacy First payment, subject to also achieving the relevant volume of clinical pathway consultations, from June 2025, pharmacies also need to be registered to provide the Hypertension Case-Finding Service (HCFS) and Pharmacy Contraception Service.
Further bundling phases are planned to: deliver at least one Ambulatory Blood Pressure Monitoring (ABPM) provision per month; and provide a specified number of contraception consultations each month. However, these have currently been delayed.
Note, due to other changes, the above requirements related to registration to provide the HCFS and the provision of at least one ABPM per month will not apply to Distance Selling Pharmacies (see further information in the Regulatory changes section below).
DHSC has also pledged to review delivery and capping of Pharmacy First and other services.
Pharmacy First service webpage
Pharmacy First: Changes to the claim period
Pharmacy First: Summary of changes from 1st June 2025
ABPM bundling requirement to be delayed
Pharmacy Contraception Service
The consultation fee for both initiation and repeat supplies of contraception increase to £25.
Suitably trained and competent Pharmacy Technicians will also be able to provide the service, supporting greater use of skill mix by pharmacy owners, where that fits within their business plans.
From October 2025, subject to the introduction of IT updates, the service will be expanded to include Emergency Contraception (EC), with a fee of £20 per consultation, plus the cost of any EC provided to the patient.
Pharmacy Contraception Service (PCS) webpage
Hypertension Case-Finding Service
The service specification will be updated to clarify patient eligibility requirements, e.g. where people request frequent measurement of their blood pressure (which is outside the scope of the service) and groups of patients that general practices can appropriately refer to the service for clinic checks.
Following changes to the VAT regulations, the service specification was changed to allow suitably trained pharmacy staff to provide the service. Accordingly, from April 2025 the fee for the clinic blood pressure check is adjusted to £10.00 per consultation.
To support the aim to provide more ABPM consultations, the fee for ABPM provision increases to £50.85 from April 2025.
NHS England will also consider whether alternative approaches to ABPM can be taken to support the potential diagnosis of hypertension, where the patient does not wish to have ABPM.
Hypertension Case-Finding Service webpage
New Medicine Service (NMS)
The payment structure for NMS is simplified to a £14 fee for each Intervention or Follow up consultation provided to the patient, i.e. a total fee of £28 will be paid if the pharmacy has done both the Intervention and Follow up consultations. Associated changes will be made to the Manage Your Service (MYS) claiming module.
From 1st October 2025, the service will also be expanded to include depression within the conditions and associated medicines covered by the service. There will be no mandatory training, but a related training programme on consulting with people with mental health problems is included in the Pharmacy Quality Scheme (PQS).
New Medicines Service (NMS) webpage
NMS: Making your end of month claim
Smoking Cessation Service
Skill mix changes will be introduced to the Smoking Cessation Service, to allow suitably trained and competent staff to provide the service, alongside pharmacists and pharmacy technicians.
PGDs will also be introduced to enable provision of Varenicline and Cytisinicline (Cytisine) under the service by both suitably trained and competent pharmacists and pharmacy technicians.
Both changes will require developments to IT systems and the date from which the changes will apply will be announced in due course.
A smaller than usual PQS is running in 2025/26, worth £30 million, with many of the elements repeating those in previous schemes to support the ongoing embedding of these quality improvements into pharmacy practice.
An Aspiration payment of 75% of the overall points value (circa £2,300 per pharmacy aspiring to undertake the whole scheme) will be available to claim in May for payment on 1st July 2025.
Contractual easements
- Clinical audits: During 2025/26, there is no requirement to complete a nationally chosen or pharmacy owner selected clinical audit.
- Health campaigns: During 2025/26, pharmacies only have to take part in a maximum of two national health campaigns and two campaigns selected by their Integrated Care Board (ICB).
- Practice leaflets: The requirement to produce a practice leaflet will be removed.
- References for new staff: The requirement to seek references for staff involved in NHS services will be removed.
- Patients signing prescription declarations: The requirement for patients that pay an NHS prescription charge to complete and sign the declaration on the rear of the prescription form or EPS token will be removed.
- NHS Profile Manager: We will work with NHS England to seek to ensure pharmacy owners’ NHS website and Directory of Services (DoS) Profiles within NHS Profile Manager are comprehensive and accurate.
DSP market entry to close plus core opening hours and other regulatory changes
Briefing 013/25: Regulatory Changes in June 2025 – DSPs, Opening Hours, etc.
Amendment of core opening hours
These regulatory amendments should enable pharmacy owners to change their opening hours to days and times that better serve their patients and likely users of the pharmacy, and in some cases, close at quiet times or out-of-hours. The amendments should also support pharmacies with operational and capacity issues. The Pharmacy Manual will be revised accordingly.
Core opening hours information
DSP market entry to close plus core opening hours and other regulatory changes
Briefing 013/25: Regulatory Changes in June 2025 – DSPs, Opening Hours, etc.
Distance Selling Premises (DSP) pharmacies
Regulations will be amended so that DSPs will no longer be able to provide Advanced and Enhanced services to patients on the pharmacy premises. Where the service specification for individual services allows remote consultations to be provided or off-site provision of a service, that will still be possible for all pharmacies, including for DSPs. This is likely to be effective on/from October 2025, after the PLPS regulations have been amended.
The DSP market entry exemption will also be closed. From 23rd June 2025, no new DSP applications can be accepted/are permitted.
Distance selling pharmacies webpage
DSP market entry to close plus core opening hours and other regulatory changes
Briefing 013/25: Regulatory Changes in June 2025 – DSPs, Opening Hours, etc.
NMS change
The service requirements for NMS will be changed to state/clarify that the service cannot be subcontracted to another provider. This will stop NMS being provided via a remote consultation with the patient by a pharmacist working off the pharmacy premises who is not employed by the pharmacy owner. This change will only be effective after the Directions for the service have been amended.
The Government also made a number of further commitments within its final offer.
Key commitments
- Crucially, the Government recognises the funding gap that remains for community pharmacy – given the findings of the Economic Analysis undertaken by Frontier Economics for NHS England – and that this settlement is a first step towards sustainability.
- A commitment to continuing to work with us to set out a sustainable funding and operational model to underpin the sector’s contribution to healthcare.
- A pledge to review both Pharmacy First delivery and the operation of the margin system.
- Confirmation that points raised in the discussions (including the Economic Analysis) will inform the Government’s Comprehensive Spending Review.
- Pledge to begin 2026/27 negotiations shortly after the summer when the current Spending Review process has concluded.
Funding and reimbursement
- Commitment to improving the medicine margin survey.
- Consideration of further strategies to stabilise Category M.
- Examination of ways to speed up Category M reimbursement price setting arrangements and change Category C price setting.
- Exploration of the impact of prescribing activities (e.g. Branded Generics) on medicine margin.
- Adoption of appropriate actions arising from the RPS Medicines shortages: Solutions for Empty Shelves report.
- Consideration of supporting earlier payment for dispensing (on the 1st instead of 12th of the month) but with a wider ambition to redesign the whole payment timetable to reduce complexity.
Services
- Further consideration of the use of caps, where required, to provide equity of access to funding for the clinical services.
- A pledge to conclude development of MYS APIs for all clinical services.
CPCF Roadshow
In April 2025 a series of online and in-person events were held to support pharmacy owners and their teams to understand the new funding and contractual arrangements.
A recorded version of the presentation is now available to watch on-demand.
For external audiences
Community Pharmacy England is continuing our political influencing campaign to gain wide and vocal support from MPs and Peers from across all parties, and to ask for their help in pressing Government to act to protect our community pharmacies for the long-term. LPCs and pharmacy owners are asked to support this work. In the first instance you may like to consider writing to MPs or hosting pharmacy visits for them using our two updated guidance documents:
We have also produced a number of other resources which may help in explaining this settlement to external audiences, such as MPs or ICBs:
- CPCF Settlement Announcement Briefing
- Summary of the independent Economic Analysis
- Animation
- Infographic Summary
For more information on this topic please email comms.team@cpe.org.uk