Pharmacy First service
Published on: 16th November 2023 | Updated on: 19th November 2025
This webpage provides information on the Pharmacy First service, which commenced on 31st January 2024.
The service was announced as part of an an agreement setting out how the £645 million investment pledged within the Delivery plan for recovering access to primary care would be used to support community pharmacy services.
The two previous elements of the Community Pharmacist Consultation Service (CPCS) were incorporated into the Pharmacy First service.
If you work in a general practice visit our Pharmacy First: Information for GP practice teams webpage
If you are a non-healthcare professional visit our Information on national pharmacy services webpage
Latest update
ESPAUR report provides insight into antimicrobial supply from pharmacies
The UK Health Security Agency has published the English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) report for 2024/25.
This year, the report includes data on antibiotics supplied to patients following a Pharmacy First clinical pathway consultation. This data is taken from the ePact2 antimicrobial stewardship Pharmacy First dashboard.
Updated clinical pathways, protocol and PGDs for Pharmacy First
The updated Pharmacy First clinical pathways, protocol and Patient Group Directions (PGDs) should be used by pharmacy teams from 1st October 2025.
NHS England published on their website the final updated clinical pathways, protocol and PGDs, as well as an updated master PGD authorisation sheet, which pharmacists can choose to sign instead of having to sign each individual PGD.
Directed services can no longer be provided at distance selling premises (DSP) pharmacies
From 1st October 2025, DSP pharmacies can no longer provide Directed services (Advanced, National Enhanced and Enhanced Services)* face-to-face with the patient at the pharmacy premises. This means they can no longer provide the Urgent supply of medicines/appliances strand or the Minor illness strand of the Pharmacy First service face-to-face with the patient at the pharmacy premises.
DSP pharmacies can now only provide Directed services remotely from the DSP pharmacy premises, similar to the delivery of Essential services or if the service specification permits, face-to-face with the patient off-site.
Read more about the changes of provision of services at DSP premises
* DSP pharmacies can continue to provide COVID-19 and Flu vaccination services at the pharmacy premises, as part of an Advanced, National Enhanced, or Enhanced service, until 31st March 2026.
ABPM bundling requirement to be delayed
DHSC, NHS England and Community Pharmacy England have agreed that the requirement to provide one Ambulatory Blood Pressure Monitoring (ABPM) consultation per month as part of the ‘bundling’ requirements to achieve a Pharmacy First fixed monthly payment will not go ahead from 1st October 2025 as originally planned.
Read more about the decision to delay the ABPM bundling requirement
Click on a heading below for more information
Community Pharmacy England made a proposal to the Department of Health and Social Care and NHS England for a Pharmacy First service back in March 2022 and followed up on our bid with an extensive influencing campaign to build wider support for the proposal from stakeholders and influencers.
The Pharmacy First service, which commenced on 31st January 2024, is a crucial first step in recognising and properly funding the enormous amount of healthcare advice that community pharmacies provide to the public every day and in establishing and funding community pharmacy as the first port of call for healthcare advice.
What does the service involve?
The Advanced service involves pharmacists providing advice and NHS-funded treatment, where clinically appropriate, for seven common conditions (age restrictions apply):

Consultations for these seven clinical pathways can be provided to patients presenting to the pharmacy as well as those referred electronically by NHS 111, general practices and others.
The service also incorporates the elements of the Community Pharmacist Consultation Service, i.e. minor illness consultations with a pharmacist and the supply of urgent medicines (and appliances), both following an electronic referral from NHS 111, general practices (urgent supply referrals are not allowed from general practices) and other authorised healthcare providers (i.e. patients are not able to present to the pharmacy without an electronic referral).
In the clinical pathway consultations with a pharmacist, people with symptoms suggestive of the seven conditions will be provided with advice and will be supplied, where clinically necessary, with a prescription-only treatment under a Patient Group Direction (PGD) or in one pathway, an over-the-counter medicine (supplied under a clinical protocol), all at NHS expense.
In the future, we hope that independent prescribers will be able to use their skills to complete episodes of care within the service, without the need for a PGD. However, for the time being, all pharmacists providing the service must use the PGDs and clinical protocol.
The service requirements are included in the service specification and the associated clinical pathways.
Download the service specification and clinical pathways
Patient Group Directions
The 23 patient group directions (PGD) and one protocol for the service authorise supply of medicines at NHS expense.
Download the PGDs and protocol
Master PGD and Protocol authorisation sheet
Pharmacists working under the PGDs and protocol and an authorising manager need to sign them before their use. This master authorisation sheet can be used to sign/authorise all 23 PGDs and the protocol in one document.
Drug Tariff
The Drug Tariff determination sets out the detail of the funding for the service (see also the Funding and claiming payment section below) and the Secretary of State Directions provide the legal basis for the provision of the service:
Drug Tariff determination and Secretary of State Directions for the Pharmacy First service
Please note, the Drug Tariff Determination for Pharmacy First has been updated since inital publication therefore the latest version of the Drug Tariff should be viewed for up-to-date information.
Pharmacy owner implementation checklist: Pharmacy First service
This checklist details the actions pharmacy owners need to undertake to prepare to provide the Pharmacy First service.
Pharmacist implementation checklist: Pharmacy First service
This checklist provides suggested actions that pharmacists need to undertake to prepare to provide the Pharmacy First service.
Webinars
In late 2023 and early 2024, Community Pharmacy England hosted a series of webinars to help pharmacy owners and their teams to prepare for the new Pharmacy First service, and changes to the PCS and Hypertension Case-Finding Service.
There were two webinars on the Pharmacy First service:
Pharmacy First: Getting to know the service – this webinar provided the initial launch information for the Pharmacy First service, outlining the core
Download the slides from the webinar
Pharmacy First: Getting ready for launch – this webinar focused on how to prepare for the service’s launch, building on the content of the earlier webinar and providing additional practical information.
Download the slides from the webinar
Consultation room
Pharmacies must have a consultation room that will be used for the provision of the service which meets the requirements of the terms of service.
There must be IT equipment accessible within the consultation room to allow contemporaneous records of the consultations provided to be made within the NHS-assured Pharmacy First IT system (see below for further information on IT systems).
Providing the service via remote consultations
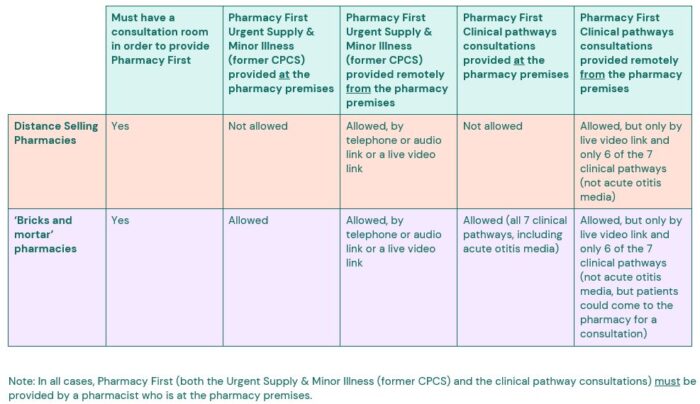
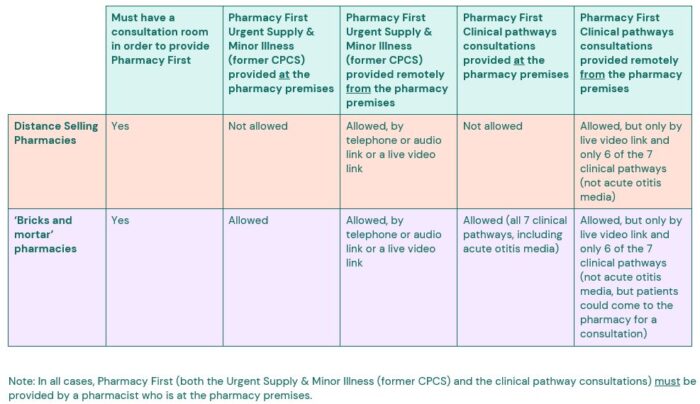
In most circumstances, the service requirements do allow remote consultations to be provided by a pharmacist who is at the pharmacy premises, but there are exceptions and specific requirements to be aware of, which are set out in the table below.
Further guidance on remote consultations
The pharmacist will also need to consider whether a remote consultation is clinically appropriate and safe to undertake.
Minor illness consultations (referrals) and urgent medicines supply consultations (referrals) can be undertaken via telephone/audio or video consultation by a pharmacist who is at the pharmacy.
Clinical pathways consultations can be conducted via good quality video consultation by a pharmacist who is at the pharmacy. Remote clinical pathways consultations can only be provided via a good quality video consultation – they cannot be provided by a telephone/audio consultation.
The acute otitis media (AOM) clinical pathway requires the use of an otoscope, so that pathway cannot not be provided via a remote consultation.
Equipment
Where ear examinations are performed within the pharmacy, the pharmacist must use an otoscope. Consequently, all pharmacies providing the service (bar DSPs) must have an otoscope.
Guidance on selecting a suitable otoscope can be found in Annex C of the service specification.
While the otoscope is the only equipment specified by the service specification, pharmacy owners may want to consider having a thermometer which can be used to measure patients’ temperatures during consultation. Tongue depressors and a small torch may also help with examination of the throat, within the sore throat pathway.
Standard Operating Procedure and Business Continuity Plan
Pharmacy owners must have a Standard Operating Procedure (SOP) for the service, which all staff participating in provision of the service must be familiar with and follow.
The SOP must include the process for escalation of any clinical and non-clinical issues identified during the provision of the service. To support this, the pharmacy must have available, signposting details for other local services, contact details for local out of hours and urgent care providers and contact details for the local Integrated Care Board (ICB).
Various pharmacy support organisations provide template SOPs which their members can personalise for use in their pharmacy. We have also produced a key contact details template for the Pharmacy First service.
Key contact details for the service (Word)
Key contact details for the service
While pharmacy owners should already have local safeguarding contacts, it is worth noting that the NHS England safeguarding app has a directory of safeguarding contacts for every local authority in England, searchable by region. It can be accessed via Apple iOS, Google Play – download it by visiting your device’s app store and searching for ‘NHS Safeguarding’.
Below is a summary template which can be used to record details on local GP practices referring into the Pharmacy First service, as well as details on other local pharmacies providing the service.
GP referrals to Pharmacy First service – summary details for local PCN (Word)
GP referrals to Pharmacy First service – summary details for local PCN (PDF)
Pharmacy owners must also ensure the service is included in their business continuity plan.
Competency and training requirements
The pharmacy owner must ensure that pharmacists providing the service are competent to do so, including the use of an otoscope (except for DSPs) and be familiar with the clinical pathways, clinical protocol and PGDs. This may involve completion of training.
The pharmacy owner must keep documentary evidence that pharmacy staff involved in the provision of the service are competent and remain up to date with regards to the specific skills and knowledge that are appropriate to their role, and to the aspects of the service they are delivering.
The Centre for Pharmacy Postgraduate Education (CPPE) has a webpage which details training resources which may help pharmacists preparing to provide the service.
CPPE have also developed, with NHS England, a Pharmacy First self-assessment framework, which pharmacists can use to assess their knowledge in relation to the service and to identify any gaps in their knowledge, which need to be filled.
CPPE Pharmacy First page (including the Pharmacy First self-assessment framework)
There are several organisations that provide Pharmacy First training and those that we have been made aware of are listed below for information. Listing below does not constitute endorsement of the course or provider by Community Pharmacy England.
Agilio iLearn Pharmacy First training
Health Academy Pharmacy First training
Tick bites/Lyme disease
While tick bites/Lyme disease is not treatable under the Pharmacy First clinical pathway for infected insect bites, with patients needing to be signposted onwards, patients may present with a tick bite with an erythema migrans (EM) rash – also known as a bullseye rash. Therefore understanding more about the signs and symptoms should help pharmacy teams recognise the symptoms and allow them to signpost patients as appropriate.
Lyme Disease UK – Resources for pharmacy teams
Lyme Resource Centre – Resources for health professionals
The prior learning, knowledge and experience of each pharmacist will vary and consequently each individual will need to reflect on their own learning needs and identify any gaps in their knowledge which they need to fill.
Selecting an IT system
As with the previous Community Pharmacist Consultation Service, an NHS-assured Pharmacy First IT system, which meets the minimum digital requirements of the service (as specified within the Community Pharmacy Clinical Services Standard and including an application programming interface (API) to facilitate transfer of data into the NHSBSA MYS portal) must be used by pharmacy owners.
When choosing an IT supplier, pharmacy owners may want to refer to the NHS CPCS IT Buyers Guide.
These IT systems allow pharmacy staff to make a clinical record for the service and the data in the record will then be used by the IT system to populate a claim for payment within the NHSBSA’s MYS portal.
The transfer of data via the API will happen throughout the month, as data is entered into the IT systems. The service provisions will then be available to view in MYS from the 1st of the following month. For example, service provisions in December will be available to view in MYS on 1st January. Pharmacy owners will then need to log into the MYS portal to check that the data matches the details in their IT system, and they will then need to submit their claim for payment.
The full dataset for the Pharmacy First service can be found in Annex B of the service specification.
The NHS-approved clinical IT system will also send messages containing a summary of the consultation to the patient’s general practice.
The following four IT suppliers worked with NHS England to develop their systems to include functionality to support the service, but over time, we expect other suppliers will add the service to their systems:
| System and supplier |
| HxConsult (Positive Solutions) |
| Pharmacy Manager (Cegedim) |
| PharmOutcomes (Pinnacle Health) |
| Sonar health (Sonar informatics) |
Read more about the IT requirements for all CPCF clinical services
Signing up to provide the service
Pharmacy owners must notify NHS England that they intend to provide the service by completion of an electronic registration through the NHS Business Services Authority’s (NHSBSA) Manage Your Service (MYS) portal
The pharmacy owner must ensure that the service is available throughout the pharmacy’s full opening hours (i.e. core and supplementary).
Verbal consent to receive the service must be sought from the patient and recorded in the pharmacy’s clinical record for the service
The patient must also be advised of the following information sharing that will take place:
- The sharing of information about the service with NHS England as part of the service monitoring and evaluation.
- The sharing of information about the service with the NHSBSA and NHS England for the purpose of contract management and as part of post-payment verification (PPV).
Annex B of the service specification includes a summary of how the data will be used by the organisations.
Resources for patients to use during/after consultations
Pharmacy First clinical pathways – online information sources for patients (Updated Oct 2025)
When pharmacists are providing a consultation for one of the seven Pharmacy First clinical pathways, there are several leaflets/websites for patients to be pointed to which are listed in the PGDs and treatment protocol.
This resource lists all the patient-facing leaflets/website links listed in the PGDs and treatment protocol, excluding the marketing authorisation holder’s patient information leaflets (hard copies will be available within the medicine’s packaging, with copies also being available from medicines.org.uk/emc).
Hyperlinks to the leaflets/websites are listed, alongside QR codes for each leaflet/website so patients can scan this to access the leaflet/website link on their mobile phones.
The following resources are available to support pharmacy teams to promote the online Pharmacy First patient survey to patients following a consultation for the Minor illness (referrals) or Clinical pathways (referrals and walk-in) strands of the service:
- Poster
The poster highlights the survey and includes a short link or QR code for the patient to scan. It could be displayed or kept in the consultation room to show to patients at the end of a Pharmacy First consultation. - Small flyers
These can be handed out to patients if they do not want to complete the survey at the end of the consultation, so they have the details of how to complete the survey later.
The short link to the survey is: bit.ly/PharmacyFirstSurvey
PDF copy of the survey questions
Accessing the patient’s record
With the patient’s consent, their GP record (e.g. via GP Connect Access Record), national care record, or an alternative clinical record for the patient, must be checked by the pharmacist unless there is good reason not to do so.
NHS England is working with Pharmacy First IT system suppliers to add GP Connect Access Record functionality to their systems. In the meantime, pharmacists providing the Pharmacy First service can continue to access elements of the patient’s GP record via the National Care Records Service.
Use of GP Connect products requires the pharmacy owner to agree to the terms of the National Data Sharing Arrangement. By accessing GP Connect products via their NHS-assured Pharmacy First IT system, the pharmacy owner will be assumed to have read, understood, and accepted the terms of the National Data Sharing Arrangement.
Communicating with GP practices following a consultation
The pharmacy must send a notification of the provision of the service to the patient’s general practice on the day of provision or on the following working day.
Where an action is required by the general practice team (such as booking the patient in for a follow up or appointment) an action message or alternative form of an Urgent Action communication (rather than the standard post event message) must be sent to the practice.
All four community pharmacy IT systems providing support for the service will automatically send standard post event messages containing details of the Pharmacy First consultation to the GP clinical IT system via a structured message, ready for a staff member at the practice to check and update the patient’s record.
This functionality – GP Connect: Update Record – means Pharmacy First post-event messages sent by pharmacy IT systems will appear in the general practice IT system’s workflow. The structured message will be provisionally held against the patient record and will be visible by people reviewing the record. A member of the practice team will need to review and accept the message. The structured message will then be ingested into the patient record without the need for transcribing or coding.
Messages will be available to anyone accessing the general practice record including patients themselves (e.g. by logging into their account on the NHS website or NHS App).
The structured message which is incorporated into the patient record will include structured data on the consultation and free text notes added by the pharmacist.
Pharmacists wanting to update their knowledge of best practice record keeping can access the CPPE Documenting in patient clinical records e-learning programme.
If the Pharmacy First IT system is unable to send a post-event message via GP Connect: Update Record it will try to send the message via NHSmail, with a summary of the consultation attached as a PDF. This is the approach which was previously used for the Community Pharmacist Consultation Service.
System supplier specific information for general practices is available via the following links:
Read more about GP Connect: Update Record
Clinical records
Details and the outcome of each consultation must be recorded in the pharmacy’s Pharmacy First IT system.
Pharmacy owners must adhere to defined standards of record keeping, ensuring the consultation record is made on the same day that it occurs unless exceptional circumstances apply.
Pharmacists wanting to update their knowledge of best practice record keeping can access the CPPE Documenting in patient clinical records e-learning programme.
Making contemporaneous records at the time of the consultation is the expectation of pharmacists providing the service. This not only meets expected professional standards, but it also supports timely provision of data to the patient’s general practice (see details of how the Pharmacy First IT system sends data to the patient’s GP practice above), which will also become available to view by other pharmacists providing a consultation to the patient, should they need to seek further support in due course.
Where the Pharmacy First IT system is unavailable due to exceptional circumstances beyond the control of the pharmacy contractor, then the consultation record must be added to the system as soon as possible after it becomes available again.
If the problem persists for a period greater than 3 working days, the contractor must notify the service commissioner (ICB) of the issue.
IT suppliers have published paper-based consultation record templates for pharmacists to use in business continuity scenarios, where the IT system is temporarily unavailable, e.g. due to a system outage or loss of internet connectivity.
Visibility of consultation records to patients
When GP Connect Update Record functionality is implemented, subject to the general practice making the record visible in online services, the Pharmacy First consultation record will be visible to the patient if they view their general practice record in online services such as the NHS app, NHS website account or GP patient apps.
Supplying medicines
If a medicine is to be supplied following an urgent medicines supply consultation or a clinical pathways consultation, the service specification requires it to be made with reasonable promptness taking into account the clinical need of the individual.
For example, supply of antivirals for the treatment of shingles for eligible patients should be made within the defined timeframes of rash onset as outlined in the clinical pathway.
The service specification notes that Distance Selling Pharmacies (DSPs) should make necessary arrangements for a prompt delivery of the item, at no cost to the patient.
If the patient needs to be referred to another pharmacy to provide the clinical pathways consultation (e.g. due to no stock of the required medicine being available at the pharmacy or the patient of a DSP needing to receive the medicine more rapidly than the pharmacy can have it delivered), no payment will be due to the referring pharmacy.
The service specification also states that to help protect NHS resources, wherever practicable, pharmacy contractors should supply the best value product to meet the clinical need of the patient.
NHS Prescription charges
The normal NHS prescription charge rules apply to medicines or appliances supplied under the service, whether via the urgent medicines supply part of the service or the seven clinical pathways.
The Pharmacy First IT system will print off a FP10DT EPS dispensing token and the patient should complete the relevant parts of the reverse of the form to claim exemption from the prescription charge or to indicate they have paid the NHS prescription charge.
The printed FP10DT EPS dispensing token must include the following information:
- Full name, address and date of birth of the patient
- Patient’s NHS number (where they have one)
- Name, strength, and form of medicines requested (using DM+D name or shortened DM+D name)
- The quantity supplied
- Date of supply
- Name and address of patient’s GP (for those who are registered with one)
- Referral ID number (if the patient was referred)
Where medicines or appliances are supplied as part of an Urgent Medicines Supply consultation, the completed dispensing tokens should be sent to the NHSBSA as part of the month-end submission, clearly separated within the batch and marked ‘PF UMS’.
Similarly, where medicines are supplied as part of a Clinical Pathway consultation, the completed dispensing tokens should be sent to the NHSBSA as part of the month-end submission, clearly separated within the batch and marked ‘PF CP’.
Temporary pharmacy closures
In the event of a temporary closure, pharmacy owners must ensure the elements of their business continuity plan related to the service are activated and the service is temporarily withdrawn.
They must inform the NHS 111 provider and local IUC CAS of the temporary withdrawal by calling the NHS Directory of Services Provider and Commissioner Helpline (0300 0200 363) as soon as possible to stop referrals being made to the pharmacy.
GP practices and UEC settings within the pharmacy’s primary care network should also be contacted to prevent them making further direct referrals.
The service commissioner (ICB) must also be informed by the pharmacy owner.
Withdrawal from the Pharmacy First service
If having registered to provide the Pharmacy First service, a pharmacy owner wishes to stop providing the service, they must notify NHS England that they are no longer going to provide the service via the MYS platform, giving at least 30 days’ notice prior to the cessation of the service. The pharmacy owner may be asked for their reason for withdrawal from the service.
After de-registering from the service on the MYS portal, pharmacy owners will not be able to re-register for one month from the final day of their 30 day’s notice. After the one month period has passed, pharmacy owners can re-register for the service via the MYS portal.
Distance selling pharmacies (DSPs) can provide the Pharmacy First service but there are some limitations on how the service is provided from a DSP with regards to the clinical pathway strand of the service:
- DSPs cannot provide consultations face-to-face (with the patient being present at the pharmacy premises).
- DSPs are limited to providing six of the seven clinical pathways consultations. The acute otitis media pathway is excluded as it requires otoscope examination of the patient’s ear and DSPs cannot provide this type of consultation with the patient being present at the pharmacy premises.
- If the patient needs to be referred to another pharmacy due to the patient requiring the medicine more rapidly than the DSP can have it delivered or if the patient needs to be referred to another pharmacy for the acute otitis media pathway (as DSPs cannot provide this pathway), DSPs cannot claim a consultation fee for this.
Other important points to note are:
- DSPs still need to have a consultation room which meets the requirements in the Terms of Service in order to provide the service. Having a consultation room is a prerequisite for the provision of the Pharmacy First service.
- Remote clinical pathway consultations must be carried out by a pharmacist, at the pharmacy premises, via a good video consultation rather than be phone. This is because the clinical pathways will often require the pharmacist to examine the patient (e.g. a rash) or examine a sample of urine, in the case of the UTI pathway. The service specification requires a live video link of sufficient quality to be used to carry out an examination, as part of the consultation. This also applies to bricks and mortar pharmacies who are providing remote clinical pathway consultations.
- The service specification notes that DSPs should make necessary arrangements for a prompt delivery of a medicine or appliance provided as part of the service, at no cost to the patient.
The various options for providing consultations are set out in the table below.
If the Pharmacy First service is to deliver the maximum possible benefit to patients, the NHS and community pharmacies, it is important that there is a strong relationship between community pharmacies and local general practices.
Such strong local relationships will give confidence to general practice teams to make referrals to the Pharmacy First and other community pharmacy services wherever appropriate for patients.
We all know achieving long-term changes in practice can take time and consequently the work to embed referrals from general practice to Pharmacy First will in most cases need to be sustained over several months or perhaps longer.
We have received positive feedback from many LPCs and pharmacy teams about how local community pharmacy/general practice relationships are driving a good volume of referrals and benefits to patients. However, some pharmacy teams are experiencing low levels of referrals or none at all.
Previous experience from the rollout of GP referrals to the Community Pharmacist Consultation Service is that sustained effort may be required to ensure that referrals are made and continue to be made over the following months.
To support pharmacy owners, their teams and LPCs to keep engaging with local general practice colleagues, we have a range of resources available:
Pharmacy First checklist – Promoting the service to your GP practice
This checklist provides suggested actions that pharmacy owners and their teams can choose to undertake to help promote the Pharmacy First service to their local GP practice team.
Pharmacy owner template email/letter to GP practices
An email/letter introducing the Pharmacy First service.
Briefing for Local Medical Committees and general practices on the Pharmacy First service
A three-page briefing introducing the service including questions and answers for GP practice teams.
PowerPoint presentation aimed at GP practice teams
A template presentation on the service that can be used by pharmacy owners or members of their team to present to GP practice teams, for example, at a practice meeting.
PowerPoint presentation aimed at patients
A template presentation on the service that can be used to present at events such as Patient Participation Group meetings at GP practices.
Pharmacy First template PowerPoint presentation aimed at Local Medical Committees and general practice colleagues – for use by LPCs
A template presentation on the service that can be used by LPCs to present to Local Medical Committees and general practice colleagues.
Template copy for websites or newsletters aimed at the public
This document contains content to promote the service to the public on GP practice websites or in their patient newsletter.
LPCs and pharmacy teams are encouraged to share the below animation and infographic with local GP practices, LMCs, PCNs and ICBs to improve understanding and engagement with the GP electronic referral pathway into the Pharmacy First service in their areas. You can show the animation at meetings directly from the Community Pharmacy England website, but if you need access to a downloadable version, please email: comms.team@cpe.org.uk
Watch the animation:
Pharmacy First: What GPs need to know infographic
Download this folder that contains the following resources:
- Clip 1: Introducing the service
- Clip 2: How the service works
- Clip 3: The value of the service
- Screenshots
- Social media tiles
- Suggested tweets/posts
We also have a page on our website aimed at GPs and their teams: Visit the Pharmacy First: Information for GPs webpage.
NHS funding to support local work with Primary Care Networks
Some of the funding allocated to the Pharmacy First service within the Primary Care Recovery Plan is being used to support local implementation of the service (and also the Pharmacy Contraception Service and the Hypertension Case-finding Service).
The funding, which was announced at the end of May 2024, will be used to support work with general practices within a Primary Care Network (PCN). Integrated Care Boards and Local Pharmaceutical Committees (LPC) are currently working together to start to implement this approach at a local level. Please contact your LPC to find out how this is progressing in your area.
Community Pharmacy England resources
We have developed a range of materials including posters, social media assets and an animation which pharmacy owners can use to promote the service to patients.
Our shared folder (link below) allows you to download the latest versions of the following resources:
- Posters for display within pharmacies and for more general use (e.g. in general practice waiting rooms);
- Social media tiles and suggested social media posts about Pharmacy First;
- Videos and digital screen graphics;
- Small flyers about Pharmacy First; and
- Template local press release for Pharmacy First launch.
Download here: Pharmacy First promotional resources
Animation for patients
The animation for patients provides clear and concise information about the Pharmacy First service, highlighting the seven conditions and the eligible age ranges within the clinical pathways consultations and explaining how patients can access those.
Pharmacy owners and their teams can use the animation to communicate the benefits and scope of the Pharmacy First service to their patients. For example, the animation can be linked to in pharmacy social media content and you can download a copy to play on digital screens in pharmacies. Similarly, general practices could be encouraged to use the animation on digital screens in their practice waiting areas.
Watch the animation:
Two shorter clips are also available on YouTube:
How the Pharmacy First service works
The value of the Pharmacy First service
Open this folder to download the following resources:
- Full animation
- Full animation with subtitles
- Clip 1: About the service and how it works
- Clip 2: The value of the service
- Social media cards
- Suggested tweets/posts
We have incorporated all of the above resources into a Pharmacy First checklist so pharmacy owners can work through the checklist to see if there are any additional activities that they or their teams could participate in to promote the service to the public:
Pharmacy First checklist: Promoting the service to patients
NHS England resources
NHS England has relaunched their Pharmacy First public-facing campaign.
Minor revisions have been made to the original campaign materials used earlier this year, including additional information on the age criteria for the clinical pathways.
The campaign materials are available on the Department of Health and Social Care’s Campaign Resource Centre website and include:
- A campaign toolkit;
- Social assets; and
- Posters.
Community Pharmacy England and Healthwatch England launched an online Pharmacy First patient survey in November 2024 that pharmacy owners can direct patients to after receiving the service.
The aim of this collaboration is to collect patient feedback on the service to help inform service improvements and to help to quantify the value of the service to the public.
Pharmacy teams providing Pharmacy First are asked to help promote the survey using the resources we have developed. To encourage as many responses as possible, the survey has been designed to be quick and easy to complete; during testing, most patients took around two minutes to complete it.
Who can use the survey?
We would like all pharmacies providing the Pharmacy First service to help gather valuable public feedback, by asking patients to complete the survey following a consultation for the Minor illness (referrals) or Clinical pathways (referrals and walk-in) strands of the service.
The survey is not for use where patients have used the Urgent supply of medicines / appliances strand of the service.
Why should we ask patients to complete the survey?
Use of the survey is optional, but we encourage pharmacy owners and their teams to consider offering it to patients for several reasons, including:
- Helping to gather important data on patients’ experience of using the service;
- Feeding into the national evaluation of the Pharmacy First service, and the results will be shared with the Department of Health and Social Care and NHS England;
- Supporting Community Pharmacy England and Healthwatch England’s national work, and local data can be shared with local Healthwatch organisations and Local Pharmaceutical Committees (LPCs) to inform their discussions on the service at a local level; and
- Reinforcing Community Pharmacy England’s communications and public affairs work to demonstrate the value of the Pharmacy First service.
We publish a national summary of survey results below.
When should I ask patients to complete the survey?
Ask patients if they would be willing to complete the survey at the end of their Pharmacy First consultation (consultations for the Minor illness or Clinical pathways stands of the service).
If the Pharmacy First consultation was for a patient who cannot complete the survey (for example, a young child), the patient’s representative can complete the survey, but the answers should be based on the Pharmacy First consultation that the patient or their representative received from the pharmacy.
The survey will remain open until at least the end of 2025.
Promoting the feedback survey
We have produced the following resources to support pharmacy teams promoting the survey to patients:
- Poster
The poster highlights the survey and includes a short link or QR code for the patient to scan. It could be displayed or kept in the consultation room to show to patients at the end of a Pharmacy First consultation. - Small flyers
These can be handed out to patients if they do not want to complete the survey at the end of the consultation, so they have the details of how to complete the survey later.
The short link to the survey is: bit.ly/PharmacyFirstSurvey
PDF copy of the survey questions
Survey results
The following dashboard includes a summary of the responses to the survey received up until 30th October 2025. As more survey responses are received, the dashboard will be updated.
Funding for the clinical pathways consultations within the new service comes from the new investment, which is outside of the Community Pharmacy Contractual Framework (CPCF) funding (‘the global sum’).
Consultation fee
Pharmacies were paid £15 per completed consultation until 31st March 2025. From 1st April 2025, the consultation fee for Minor illness and Clinical Pathway consultations increased to £17 (from £15). The fee for Urgent supply consultations remains at £15.
There are many different scenarios which can occur within the service, so to help pharmacy owners and their teams know when you can make a claim for a payment, we have published a resource to assist with this. It lists the different scenarios, whether you need to make an entry in your Pharmacy First IT system for that scenario and whether you can claim payment:
The Pharmacy First service – When can you claim?
Monthly fixed payment
In addition to the consultation fee, a monthly fixed payment of £1,000 will be paid to pharmacy owners who meet a minimum activity threshold of clinical pathways consultations (the threshold will increase over time as set out below).
Achieving the thresholds for the monthly Pharmacy First payment has been an ongoing matter of great concern for pharmacy owners and Community Pharmacy England. There have been three agreed changes to the original thresholds, which were secured following Community Pharmacy England representations to the Department of Health and Social Care (DHSC) and NHS England. The table below shows the current thresholds that need to be achieved.
| Month | Minimum number of clinical pathways consultations |
| February 2024 | 1 |
| March 2024 | 5 |
| April 2024 | 5 |
| May 2024 | 10 |
| June 2024 | 10 |
| July 2024 | 10 |
| August 2024 | 15 |
| September 2024 | 20 |
| October 2024 | 20 |
| November 2024 | 20 |
| December 2024 | 20 |
| January 2025 | 25 |
| February 2025 | 25 |
| From March 2025 onwards | 30 |
Only clinical pathway consultations that cross the gateway point and reach an outcome set out in the pathway (without onward referral to another pharmacy), will count towards meeting the monthly minimum number of consultations for the block payment.
Addition of an intermediary monthly payment band
From 1st June 2025, a banded approach will be added to the monthly payment:
- £500 for those providing 20-29 Clinical pathways consultations within a month; and
- £1000 for those pharmacies that provide 30 or more Clinical pathways consultations within a month.
To accommodate that change to the monthly payment within the NHSBSA’s systems, for Pharmacy First consultations provided from 1st June 2025, pharmacy owners will need to claim for the consultations within one month from the end of the month in which they were provided.
For example, Pharmacy First consultations provided in June will need to be claimed on MYS by the last day of July.
The recent change to allow an additional twelve months to claim payment where an issue with IT systems prevented the submission of a claim will remain.
‘Bundling’ requirements for the monthly payment
It was previously announced that ‘bundling’ requirements would be introduced from April 2025 requiring pharmacy owners to provide the HCFS and PCS in order to receive the Pharmacy First monthly payment, when they also meet the monthly volume target.
We have agreed revisions to this plan with a phased introduction of ‘bundling’ requirements. To receive the monthly Pharmacy First payment, subject to also achieving the relevant volume of clinical pathway consultations:
- From June 2025, pharmacies will need to be registered to provide the PCS and HCFS;
- From October 2025, in addition they must deliver at least one Ambulatory Blood Pressure Monitoring (ABPM) provision per month – please note, this bunding requirement has been delayed; and
- From March 2026, a specified number of contraception consultations, including emergency contraception consultations, will also need to be provided each month. The specified number will be agreed by Community Pharmacy England, DHSC and NHS England in due course.
In recognition of forthcoming changes to the rules around provision of Advanced and Enhanced services to patients present on the premises of Distance Selling Premises pharmacies (DSPs) the above requirements related to registration to provide the HCFS and the provision of at least one ABPM per month will not apply to DSPs.
Caps on the provision of Pharmacy First clinical pathways consultations
In April 2024, an initial cap of 3,000 consultations per month per pharmacy was put in place. From 1st October 2024, new caps were introduced based on actual provision of clinical pathways consultations, with any unused activity rolling forward to subsequent quarters of that financial year.
From April 2025, news caps were introduced, with a monthly allocation which will be updated each month to reflect actual delivery of the service by individual pharmacies. Any activity above the monthly cap will not receive the £17 per consultation fee.
The Pharmacy First Clinical Pathways band assignments and monthly caps are published on the NHSBSA website.
The list published by NHSBSA indicates the band assignment and monthly cap for each pharmacy by ODS code.
If a pharmacy ODS is not included in the list, the pharmacy is automatically considered to be in Band 1 (the lowest band).
Claiming payments
Data from the Pharmacy First IT system will be submitted to the MYS portal via an application programming interface and will be used by the NHSBSA to populate a payment claim within the MYS portal.
The pharmacy owner needs to review this payment claim and then submit it via the MYS portal by the 5th day of the month following the month in which the chargeable activity was provided. To align with the payment timetable highlighted in Table 3 in Part I of the Drug Tariff, where one or more bank holidays occur within the first five days of the following month, claims for payment should be submitted by the 6th of that month.
Before 1st June 2025, late submissions were accepted if made within three months of the date by which the claim should have been submitted. From 1st June 2025, late submissions will only be accepted if they are made by the final day of the month following the month in which the Pharmacy First consultation was conducted. For example, claims for consultations provided in June 2025 will need to be submitted by 11.59pm on 31st July 2025.
From 1st June 2025, this change will also impact the claim windows for Pharmacy First consultations conducted from March 2025 onwards. Therefore claims for consultations carried out in March, April and May 2025 must be claimed by 11:59pm on Monday 30th June 2025.
Later claims will not be paid, unless the submission of a claim was delayed by IT issues outside the pharmacy owner’s control (such as issues with the NHS approved API system used by the pharmacy owner or with the MYS portal). Such claims will be accepted outside the usual grace period within twelve months of the date by which the claim should have been submitted. This is subject to the NHSBSA receiving evidence of the IT issue, and only if investigation finds that the evidence demonstrates that the IT issue was outside the control of the pharmacy owner, and it delayed the claim submission.
Claims may be investigated if provision is outside of service requirements
New wording was added to Part VIC of the February 2025 Drug Tariff to advise that where claims are submitted for Pharmacy First and the data provided indicates the service was not provided in accordance with the appropriate Patient Group Direction (PGD) or service specification, the payments may be withheld by the NHS Business Services Authority while the claims are investigated.
Examples of this include:
- If an excessive quantity of medicine has been supplied, for example, outside that stipulated in the PGD;
- A patient was outside the age range of the PGD, for example, a woman aged 65 or over for an Uncomplicated urinary tract infection; or
- An acute otitis media pathway was provided by a distance selling pharmacy.
Following the outcome of the investigation, payments will only be made to pharmacy owners ifthe pharmacy owner provides sufficient evidence to show that the supply was in accordance with the appropriate PGD and service specification.
Schedule of payments
As a result of the launch of the Pharmacy First service the method and quantum of pharmacy owner payments will change. To reflect this, NHSBSA has made changes to the Schedule of Payments and E-Schedules to provide more detail for pharmacy owners. As part of this exercise, broader changes were also made for consistency and to provide as much detail as possible of the breakdown of payments.
Example Pharmacy First Schedule of Payments
Example Pharmacy First E-Schedule (ZIP file)
This Zip file contains:
- E-Schedule Map (Excel)
- Sample E-Schedule (DAT)
Guidance and resources for pharmacy owners
Pharmacy owner implementation checklist: Pharmacy First service
This checklist details the actions pharmacy owners need to undertake to prepare to provide the Pharmacy First service.
The following briefings provide summary information about what the overall agreement on the Delivery plan for recovering access to primary care negotiations means in practice.
Briefing 029/23: Recovery Plan agreement – Summary and FAQs for pharmacy owners and LPCs
Key contact details for the service (Microsoft Word)
Key contact details for the service (PDF)
Pharmacy owners must have available, signposting details for other local services, contact details for local out of hours and urgent care providers and contact details for the ICB. The above resource can be used to list all of the key contacts for the service.
While pharmacy owners should already be aware of local safeguarding contacts, it is worth noting that the NHS England safeguarding app has a directory of safeguarding contacts for every local authority in England, searchable by region. It can be accessed via Apple iOS, Google Play – download it by visiting your device’s app store and searching for ‘NHS Safeguarding’.
Below is a summary template which can be used to record details on local GP practices referring into the Pharmacy First service, as well as details on other local pharmacies providing the service.
GP referrals to Pharmacy First service – summary details for local PCN (Word)
GP referrals to Pharmacy First service – summary details for local PCN
Guidance for pharmacists
Pharmacist implementation checklist: Pharmacy First service
This checklist provides suggested actions that pharmacists need to undertake to prepare to provide the Pharmacy First service.
Resources to use during/after consultations
Pharmacy First clinical pathways – online information sources for patients (Updated Oct 2025)
When pharmacists are providing a consultation for one of the seven Pharmacy First clinical pathways, there are several leaflets/websites for patients to be pointed to which are listed in the PGDs and treatment protocol.
This resource lists all the patient-facing leaflets/website links listed in the PGDs and treatment protocol, excluding the marketing authorisation holder’s patient information leaflets (hard copies will be available within the medicine’s packaging, with copies also being available from medicines.org.uk/emc).
Hyperlinks to the leaflets/websites are listed, alongside QR codes for each leaflet/website so patients can scan this to access the leaflet/website link on their mobile phones.
The Pharmacy First service – When can you claim?
There are many different scenarios which can occur within the service, so to help pharmacy owners and their teams know when you can make a claim for a payment, we have published a resource to assist with this. It lists the different scenarios, whether you need to make an entry in your Pharmacy First IT system for that scenario and whether you can claim payment.
The following resources are available to support pharmacy teams to promote the online Pharmacy First patient survey to patients following a consultation for the Minor illness (referrals) or Clinical pathways (referrals and walk-in) strands of the service:
- Poster
The poster highlights the survey and includes a short link or QR code for the patient to scan. It could be displayed or kept in the consultation room to show to patients at the end of a Pharmacy First consultation. - Small flyers
These can be handed out to patients if they do not want to complete the survey at the end of the consultation, so they have the details of how to complete the survey later.
The short link to the survey is: bit.ly/PharmacyFirstSurvey
PDF copy of the survey questions
Information for pharmacy teams
Briefing 010/24: Briefing for pharmacy teams – the Pharmacy First service
This Briefing provides information for pharmacy teams on the Pharmacy First service.
Information for Local Medical Committees and general practices
Pharmacy First checklist – Promoting the service to your GP practice
This checklist provides suggested actions that pharmacy owners and their teams can choose to undertake to help promote the Pharmacy First service to their local GP practice team.
Pharmacy owner template email/letter to GP practices
Pharmacy First template PowerPoint presentation aimed at GP practice teams
A template presentation on the service that can be used by pharmacy owners or members of the team to present to GP practice teams, for example, at a practice meeting.
PowerPoint presentation aimed at patients
A template presentation on the service that can be used to present at events such as Patient Participation Group meetings at GP practices.
Pharmacy First template PowerPoint presentation aimed at Local Medical Committees and general practice colleagues – for use by LPCs
A template presentation on the service that can be used by LPCs to present to Local Medical Committees and general practice colleagues.
Template copy for websites or newsletters aimed at the public
This document contains content to promote the service to the public on GP practice websites or in their patient newsletter.
LPCs and pharmacy teams are encouraged to share the below animation and infographic with local GP practices, LMCs, PCNs and ICBs to improve understanding and engagement with the GP electronic referral pathway into the Pharmacy First service in their areas. You can show the animation at meetings directly from the Community Pharmacy England website, but if you need access to a downloadable version, please email: comms.team@cpe.org.uk
Watch the animation:
Pharmacy First: What GPs need to know infographic
Download this folder that contains the following resources:
- Clip 1: Introducing the service
- Clip 2: How the service works
- Clip 3: The value of the service
- Screenshots
- Social media tiles
- Suggested tweets/posts
Visit the Pharmacy First: Information for GPs webpage
Other resources for Local Pharmaceutical Committees
Pharmacy First template PowerPoint presentation aimed at pharmacy owners and teams – for use by LPCs
A template presentation on the service that can be used by LPCs to present to pharmacy owners and their teams.
Pharmacy First template PowerPoint presentation aimed at other external audiences – for use by LPCs
A template presentation on the service that can be used by LPCs to present to other external audiences.
Nitrofurantoin analysis
The dashboard contains NHSBSA PCA data from May 2023 to April 2024 for the dispensing in the community of solid dosage forms of Nitrofurantoin. It also contains data from the same source on the supply of Nitrofurantoin via the Pharmacy First clinical pathways (just for February to April 2024).
Promotion of the service to patients
Pharmacy First promotional resources
NHS England ‘Think Pharmacy first’ campaign materials
Pharmacy First checklist: Promoting the service to patients
Since the launch of the service, Community Pharmacy England and NHS England have published a number of resources (linked to above) to support pharmacy owners and their teams to promote the Pharmacy First service.
We have incorporated all of these into a Pharmacy First checklist so pharmacy owners can work through the checklist to see if there are any additional activities that they or their teams could participate in to promote the service to the public.
Pharmacy First template PowerPoint presentation aimed at patients
A template presentation on the service that can be used to present at events such as Patient Participation Group meetings at GP practices.
Template copy for websites or newsletters aimed at the public
This document contains content to promote the service to the public, for example on GP practice websites or in their patient newsletter.
NHS England Pharmacy First leaflet (easy read)
Promotion of the service to parents/carers through schools and nurseries
To support pharmacy owners, their teams and LPCs to engage with schools and nurseries, the following resources are available:
- Pharmacy First checklist – promoting the service to schools and nurseries
This checklist provides suggested actions that pharmacy owners, their teams and LPCs can choose to undertake to help promote the Pharmacy First service to their local schools and nurseries. - Template email/letter to schools and nurseries
A template email/letter introducing the Pharmacy First service for: - Poster
The poster could be displayed in the waiting area on noticeboards or in the teacher’s break room. These could also be printed as leaflets and included in the children’s school bags for parents/carers to see when they get home. - Template copy for school or nursery websites or newsletters
This document contains content to promote the service to parents/carers of children on websites or in newsletters. - Template email/letter from headteacher/nursery manager
A template news story that headteachers/nursery managers could send out to parents/carers about the Pharmacy First service for:
Pharmacy First Clinical pathways – medicines included in the PGDs and medicines protocol
Pharmacy First – medicines list for clinical pathway consultations (updated Oct 2025)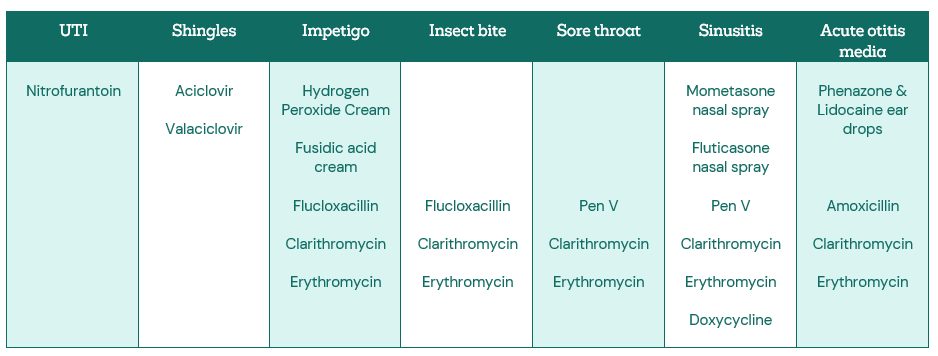
NHS England video clips
David Webb, Chief Pharmaceutical Officer, NHS England talks about the Pharmacy First service
Pallavi Dawda, Head of Delivery – Clinical Strategy, Community Pharmacy, NHS England talks about the development of the Pharmacy First service clinical pathways and PGDs
NHS England case study and podcast
West Yorkshire showcases partnership working to deliver Pharmacy First
Transforming Primary Care podcast: Pharmacy First – Reflections on the first nine months
Community Pharmacy England clinical service statistics dashboard
The dashboard presents data on the Pharmacy First service (as well as other Advanced services) at three levels (national, LPC and individual pharmacy) for each quarter. The dashboards are based on the NHS Business Services Authority’s (NHSBSA) Dispensing Contractors’ data.
NHSBSA Pharmacy First clinical pathways data
NHSBSA has created a page on their website to show the Pharmacy First clinical pathway data.
NHSBSA Dispensing contractors’ data
Data on the Pharmacy First service (as well as other Advanced services) can be found by clicking on the ‘Pharmacy and appliance contractor dispensing data’ dropdown tab.
At Community Pharmacy England, we are always keen to hear from pharmacy owners and their teams about how the provision of national pharmacy services is going, be that niggles with the way services are commissioned, a success story you want to share or something else.
Please click on the link below to share a success story where you have helped achieve a good outcome for a patient following a consultation for a national pharmacy service or to provide feedback on one of the services.
For more information on this topic please email services.team@cpe.org.uk