Community Pharmacy IT Group (CP ITG) workstream updates (archive)
Published on: 4th October 2021 | Updated on: 19th October 2023
Read more about CP ITG and its work at: the Community Pharmacy IT Group (CP ITG) webpage.
This ‘CP ITG workstream update (archive)‘ webpage sets out information following past CP ITG meetings based on past pharmacy IT bulletin.
The bulletins (including the most recent one) can also be downloaded in pdf format at the CP ITG webpage.
CP ITG has five workstream areas:
- Interoperability and security: Ensuring information about people’s health and care can be safely and securely accessed, wherever it is needed. (WS1a-1d)
- Reducing burden: Use of digital to reduce the burden on pharmacy teams, so they can focus on patients, and appropriate infrastructure for the task. (WS2a)
- Good use of digital: Support the use of digital within pharmacy to improve health and care productivity, improve patient safety outcomes and improve cooperation between pharmacy teams and the health and care system. (WS3a-3c)
- Patient and pharmacy tools: Support enabling patients to be able to choose digital tools to access medicines information and pharmacy services directly, so they can receive the best outcomes, recognising the need to also remain inclusive for all patients. (WS4a)
- Set out roadmap priorities: Development and promotion of a wider community pharmacy digital roadmap / vision. (WS5a)
Those areas have some alignment with NHSX missions. See downloadable PDF version of the full: CP ITG workstreams.
These sections below set out updates related to these workstreams based on the most recent pharmacy IT bulletin.
Community pharmacy IT developments
PSNC becomes Community Pharmacy England
Community Pharmacy England is the new name for the representative body for all community pharmacies in England – from 30th May 2023. Community Pharmacy England will continue to work closely with everyone in the community pharmacy sector. Its goals are to develop the NHS community pharmacy service, to enable community pharmacies to offer a range of services that meet the needs of their local communities and provide value and good health outcomes for the NHS and the public. Its committee is made up of representatives of pharmacy owners in England from all parts of the community pharmacy sector. The name change reflects the organisation’s current and future work. Changes have been applied to the website: cpe.org.uk (and webpage redirects are in place) and its Digital and Technology section. The email contact points for CP ITG secretariat correspondence have been updated to it@cpe.org.uk and Daniel.Ah-Thion@cpe.org.uk (email redirects are in place if the older email addresses are used).
Overview of pharmacy IT priorities overview and brief update on the IT elements proposed within the Primary Care Recovery Plan
NHS England, DHSC and the CP ITG have previously flagged the pharmacy IT priorities: PRSB Community Pharmacy Data Standard / Community Pharmacy Contractual Framework (CPCF) IT; records access; payment and data APIs; Booking and Referral Standards (BaRS); and EPS next generation. The CP ITG has continued to support these projects and Community Pharmacy England is also working with the NHS on the next steps to progress these areas. These priorities align with the CP ITG’s vision and the ‘key to the future of pharmacy IT’ infographic (which incorporates requested updates from CP ITG and pharmacy reps. The Primary Care Recovery Plan sets out digital enablers in line with these (see the IT policy: Delivery plan for recovering access to primary care section).
Establishing data flows & IT standards
Payment and data Manage Your Service (MYS) APIs for CPCF services
NHS England and Community Pharmacy England want suppliers to be given information about the service, including the IT implications and dataset requirements. The MYS API priorities were previously listed as: Pharmacy Contraception Service, Discharge Medicine Service (DMS), Blood Pressure Checking Service, New Medicine Service (NMS) and the Smoking Cessation Service. CP ITG pharmacy representatives previously reported that data entry for services such as DMS is taking a large amount of pharmacy teams. During April 2023 NHSBSA released an expression of interest for the DMS API to explore interest with the market providing this integration service. NHS England and NHSBSA had been committed to prioritising API programmes progress within 2023/24 delivery plans.
Update on Professional Record Standards Body (PRSB)’s Community Pharmacy Data Standard (CPDS)
PRSB’s Community Pharmacy Data Standard (CPDS) remains critical for enabling:
- the community pharmacy sector being able to record and transfer data in a consistent and structured way;
- suppliers to use a blueprint; and
- other parts of healthcare and the NHS from receiving information in a structured format.
NHS England commissioned PRSB to uplift CPDS. The uplift was to reflect changes to the Community Pharmacy Contractual Framework in England and for purposes of futureproofing. PRSB arranged two webinars: a supplier meeting (2nd February 2023), and a general webinar (7th February 2023). CP ITG participants were encouraged to attend these. CP ITG have also been provided with email updates about the project during the months after those. The uplift plans were set out within this slide-set. An Information Standards Notices (ISN) application was approved by Data Alliance Partnership Board (DAPB) subject to approval of the clinical safety case by the NHS England Transformation Directorate’s Clinical Safety Group (CSG) which is likely within June 2023. The ISN specifies implementation by suppliers during 2024 calendar year and compliance by end of March 2025. Implementation support for suppliers from PRSB is awaiting business case approval in NHS England. Queries relating the standard can be directed to support@theprsb.org or the PRSB Standard support query webform.
Supporting NHSmail
- Community Pharmacy England published a factsheet for community pharmacy teams explaining how to access the shared NHSmail inbox within the Outlook mobile app.
- The Virtual Visits tool provides pharmacy members with an appointments system so that they can notify patients and better manage appointments. Pharmacy teams can also use the Virtual Visits tool to conduct face-to-face or virtual patient consultations (audio or video).
- The Virtual Visits tool works in conjunction with NHSmail Microsoft Teams and the Microsoft Booking platform. To participate in the pilot, you must have an active personal NHSmail account, access to a shared NHSmail inbox, MS Teams installed on a computer or tablet and a computer or device with a webcam. Pharmacy members can now:
- register interest with taking part in the Virtual Visits pilot via this webform;
- view the one-page factsheet about How Virtual Visits works; and
- consider the guidance checklist.
NHSmail multi-factor authentication (MFA)
- MFA is already a requirement for Welsh NHSmail. CP ITG previously fed back to the NHSmail team that clear communications and proper testing should occur prior to a full roll-out of MFA across pharmacy NHSmail users. Community Pharmacy England and the NHSmail team have worked on guidance to support the testing of MFA.
- MFA will be an important development for NHSmail. It helps data to be kept within a more protected environment. It helps protect the reputation of the NHS, and the individuals and organisations that use NHSmail. It also provides increased protection against cyber-attacks. The NHSmail plan is to make MFA mandatory for all NHSmail users. The NHSmail team expect most organisations to have fully implemented MFA within January to March 2024. Mandatory rollout of MFA for the PODS NHSmail users (pharmacy, optometry, dentistry and social care, DACS, Independent Midwives, GP Locums) is currently scheduled for January 2024.
- Community Pharmacy England working with the NHSmail team has a prepared new one-page factsheet for those pharmacy NHSmail users testing MFA (or adding/removing MFA).
- Next steps:
- Pharmacy representatives can feed back about the preferred MFA options.
- Pharmacy representatives are also encouraged to urgently put themselves forward to test out MFA by using the guidance factsheet to switch MFA on. Pharmacy representatives are encouraged to submit comments to it@cpe.org.uk about piloting experiences and comments on the new guidance for MFA pharmacy testers.
Recommended minimum transfer dataset for pharmacies switching from one patient medication record (PMR) system to another
- Community Pharmacy England previously supported developing a recommended minimum dataset for cases where a pharmacy member has switched from one PMR system to another. For the sake of continuity of patient care, it is critical for some patient information to be transferred from the old to the new system.
- Community Pharmacy England has worked further with a CP ITG sub-group on the minimum agreed minimum dataset and associated transfer specification document during March-May 2023. This has resulted in the documents being iterated to 0.99 versions:
- Version 1.0 is expected to be promoted from late June 2023.
Standards
NHS England are conducting a dm+d survey about further changes to virtual medicinal product (VMP) drug forms. This survey was originally going to close in April 2023 but the close data has been extended. CP ITG suppliers in particular were (and are) encouraged to take part.
Developing robust services IT & systems
CP ITG inputs about pharmacy IT supplier development
Community Pharmacy IT Group were asked to feed into “Items for pharmacy IT supplier development” infographic. The feedback from pharmacy representatives and supplier representatives is set out on the next page. Further feedback is welcome from all pharmacy team members. Please contact it@cpe.org.uk with comments by the end of June 2023 so that your comments can be incorporated into the next iteration of the infographic.
Pharmacy IT development: technical and commercial approaches via the NHS Digital Care Services Catalogue
NHS England previously fed back it continued to explore commercial requirements and opportunities that will support both the needs of the sector and system suppliers now and in the future to support and develop an open supplier market. Currently there is not a comprehensive framework for NHS England to incentivise community pharmacy IT system suppliers to make technical developments that would align with the objectives within the NHS Community Pharmacy Contractual Framework (CPCF). NHS England are seeking to put a process and framework in place to enable this across pharmacy and other sectors. NHS England’s Transformation Directorate plans to support community pharmacy suppliers moving onto the Digital Care Service Catalogue (which is also used by GP IT Futures framework). NHS England’s Transformation Directorate hosted a kick-off call with suppliers and some Community Pharmacy IT Group representatives on 26th April 2023. A meeting recording is available for relevant participant organisations.
- A Prior Information Notice was issued to the market (including CPCS suppliers) on 1st June 2023 including:
- Digital Pathways Framework;
- Legacy Foundation Solutions Framework (periodic refresh of GP IT Futures Framework);
- Primary Care Support Services (period refresh of GPIT Futures with greater scope definition);
- Detained Estate (covers the estate in England and Wales, single clinical system);
- Research Development & Engagement (opt in Framework facilitating direct agreements between NHS England and parties); and
- Engagement with Community Pharmacy regarding CPCF Digital Service Standards & Roadmap.
- Supplier Expression of Interest (EOI) Forms were available with deadline midday 16th June. Further NHS England discussions with the community pharmacy supplier community are anticipated over June 2023 fortnight. NHS England’s Transformation Directorate are planning to publish supportive documentation for suppliers.
Pharmacy Contraception Service IT
NHS England announced that Pharmacy Contraception Service (PCS) commenced as an optional Advanced Service for community pharmacies from 24th April 2023. On 9th May 2023, the Government and NHS promised investment in community pharmacies over the next two years, part of which could support the expansion of the NHS Pharmacy Contraception – and NHS England and Community Pharmacy England are to consider the details of such an expansion.
It has been a soft launch with minimal communication to the sector and to respect the current sensitivities around workforce and financial pressures and the feedback from Community Pharmacy England on behalf of its pharmacy members.
Most engagement has been done through regional teams that are supporting pharmacy teams that opted to engage during this earlier stage of rollout. The key requirement of the specification is for the pharmacy members to use an approved IT solution (current options are the Cegedim and PharmOutcomes which are being provided free of charge until April 2024 while other IT supplier commercial models may vary). As of June 2023, 1,600 pharmacy members had registered to provide the service. The team mentioned that they have had positive feedbacks from Cegedim and PharmOutcomes, on the end-to-end API having been made available early, there were no reported IT issues and pharmacy feedback to NHS England is that they are finding the IT easy-to-use, particularly when they self-populate.
The post event message for GPs which can be automatically populated is saving time compared to what pharmacy teams had to do during the pilot.
Services IT
- NHS England announced that the way some Community Pharmacist Consultation Service GP referrals are sent by the EMIS PharmRefer product is changing.
- Pharmacy representatives that use an Point of Care vaccination system, who would like to share how these can develop etc, please email it@cpe.org.uk and you can be put forward for potential participation within an NHS user researcher project.
Urgent treatment centres and emergency departments can now refer patients to community pharmacists
NHS England update: “Urgent treatment centres and emergency departments can now start to refer patients for a consultation with a community pharmacist for a minor illness symptom or for an urgent supply of a regular medicine, using an IT solution which meets the minimum digital requirements of the service (as specified within the NHS Community Pharmacist Consultation Service Technical Toolkit). A toolkit of supporting information, including an updated CPCS specification, can assist regional and ICB teams with mobilisation plans. From 1st June 2023 in a change from the previous service specification, claims for payment should be submitted within one month of, and no later than three months from, the claim period for the chargeable activity provided.”
Digital prescriptions & services
Electronic Prescription Service (EPS)
- Pharmacy teams are encouraged to complete the EPS Paperless, Outcomes and Trackability survey (5- 7 mins). The results are feed into a study by Kinston University and will also be shared to the NHS England EPS team. Community Pharmacy England has promoted this survey.
- The NHS EPS team will be seeking more feedback from stakeholders and capturing feedback through one-to-one sessions during summer 2023 and potentially beyond. This engagement will capture further views regarding EPS trackability improvements. EPS user research team sessions will be run in a similar fashion as was done last year i.e. a remote interview and review of any prototyped screens. We’d encourage you to register interest with participating by using this signup form if you’ve not previously listed yourself: https://feedback.digital.nhs.uk/jfe/form/SV_eu4jQRNbJooQxoO.
- Business Leader reported that Titan PMR becomes first NHS accredited software for dispensing doctors.
Real Time Exemption Checking (RTEC)
- The NHSBSA continues to lead the RTEC project. The NHSBSA, DWP and the RTEC steering group plan has supported the expansion of the DWP RTEC functionality to additional pharmacy members. The group may suggest items for the RTEC development roadmap by emailing it@cpe.org.uk.
Independent prescribing IT
- The General Pharmaceutical Council (GPhC) previously consulted and reported on changes to the requirements for entry to independent prescribing courses, and the Pharmaceutical Journal reported that independent prescribing piloting was to begin across England from 2023. NHS England previously reported into the CP ITG about the plans for the pathfinder programme.
- CP ITG Chair, Matt Armstrong is taking part with NHS England’s independent prescribing pathfinders’ operational group on behalf of the CP ITG. This group will play a key role with supporting the programme and the evaluation that will inform longer term strategy for introducing independent prescribing into community pharmacy clinical services and providing input to the requirements for EPS system to support pathfinders.
- NHS England pharmacy team are awaiting the outcome of Moderation and hoping to inform Integrated Care Boards of their successful Expressions of Interest soon.
- Ppharmacy teams are encouraged to complete the Independent Prescribing Programme & IT survey (5-7 mins).
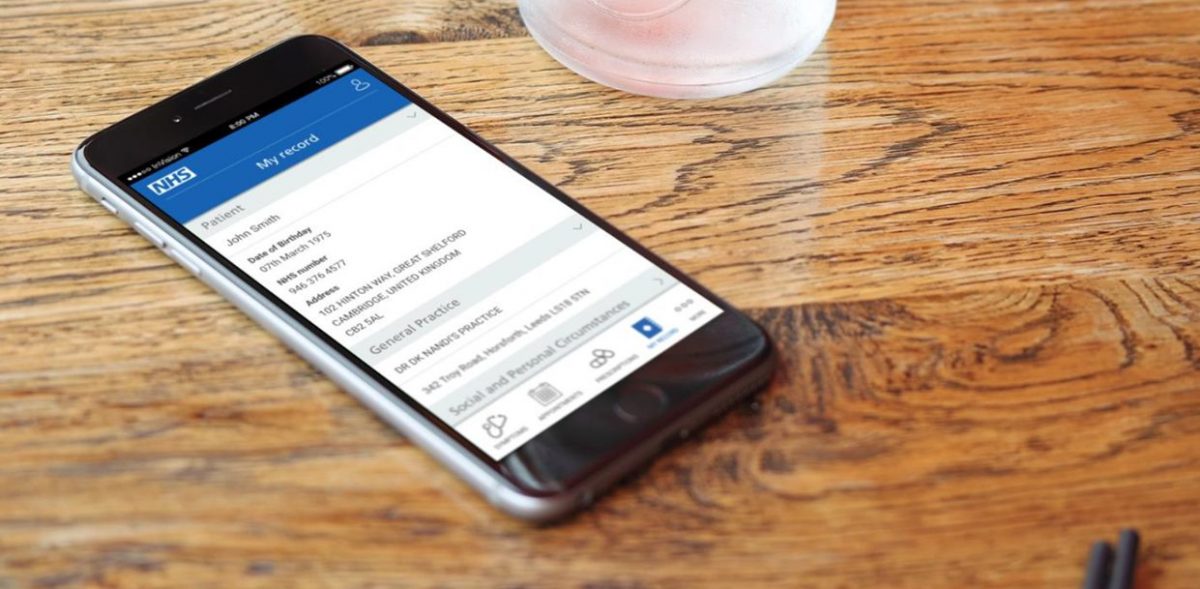
Digital first
The government has previously set targets for increasing the digital options for patients using the NHS e.g. ability to book appointments online and to order repeat prescriptions online. NHS App is one app which provides such functionality but other apps and websites aligning to relevant NHS IT standards are also increasing digital patient interactions. NHS App updates are outlined within the NHS App section below. Further workshops are to be planned regarding apps and NHS App developments. CP ITG will be invited to those. If you are use an app or provide an app to pharmacies, and would wish to take part please contact it@psnc.org.uk within June 2023 with ‘Apps event’ within the email subject title.
Patient experiences of systems and equality considerations
Case study in West Yorkshire: West Yorkshire is a multi-cultural region of England, where a diverse number of languages are spoken by people as a first language. A percentage of this demographic have a limited proficiency in English, a language that all prescriptions and pharmacy labels are printed in. NHS West Yorkshire Integrated Care System (WY ICS) & North of England Commissioning Support Unit (CSU) are supporting a pilot in which community pharmacy teams and hospital pharmacy teams can use IT to provide translated medicine dose instructions. At this time only one supplier met the criteria for initial participation within the pilot: Written Medicine. The Pharmacy Terms of Service do not set out requirements for translation activity however pharmacy teams that participate within the pilot receive the software and receive funding towards their work and costs involved. Community Pharmacy West Yorkshire are feeding into the pilot. The pilot findings are to be evaluated by a local university. Lots of patients are not taking their medicines correctly and a portion of this is likely to be due to language challenges. Pictograms/illustrations and audio files are also being added, broadening the application to meet all accessible information and reasonable adjustment needs (although this is not yet part of the pilot). The pilot areas are West Yorkshire and Harrogate – an area in which the solution will be helpful for a larger segment of patients. The pilot prioritises hospitals and community pharmacies and it will be launched from July 2023, and further volunteers will be sought. The pilot team is consulting a stakeholder group which includes Community Pharmacy West Yorkshire. The pilot may run for six months from September, depending on the uptake and other factors.
NHS App objectives
The NHS App team say their overall objectives 2023/24 are the below.
- Maximise value from the NHS App by increasing self service and self care to aim to reduce demand on the front line.
- Continue developing appointments, record access and prescriptions capabilities to keep up with policy and emerging user needs.
- Continue to develop the design and navigation of services to address user needs.
- Continue to enhance the messaging capability to improve the experience for senders and recipients.
- Ensure the NHS App team understand enough about all users’ behaviours and the full capability of the channel to help them to complete usable end to end journeys.
- Extend the integrated services available in the NHS App to support localisation and better meet users’ healthcare needs.
- Extend the underlying capabilities of the NHS App platform with a view to providing the platform capabilities for our future ambitions.
NHS App recent and future developments
The NHS App team are continuing to develop existing and future features. Selected developments are listed below. The full roadmap list is at: https://digital.nhs.uk/services/nhs-app/future-developments.
Recently completed:
- Integrated the National Booking Service so that people can book their Spring Covid vaccine booster using the app.
- Self-asserted blood pressure test results discovery, to understand what is needed to build a service that works for patients and practices.
Working on now:
- Digital Prescription Token discovery and scoping an online prescription ordering service for users without a nominated pharmacy.
- Improve the way that primary care data is sent to the app, to enable a richer, more user-centred experience. This work is often referred to as GP patient-facing APIs.
- Improve test results to allow patients to easily access and understand test results.
- Digitally requesting proxy access for adult to adults with capacity (private beta).
- Allow people to easily find and register with a GP within the app.
- Extend hospital appointment supplier integrations to give more patients access to improved secondary care appointment information.
- Simplify NHS App integrations with national services and other senders.
Working on next:
- Book and manage flu vaccinations via the app.
- Medicines A-Z from NHS App to give people easier access to information about their medications.
- Prescription order updates to users with repeat prescriptions.
- Improve hospital appointment supplier integrations to give more patients access to improved more secondary care appointment features.
- Enable people to update their postal address through the NHS App.
- Notifications relating to GP registration.
- Offering users communications about their covid vaccine appointment confirmations and reminders.
Other NHS account and NHS App updates
- Digital Health published an article on the NHS App being a critical tool in tackling the elective care backlog.
- Dan Collins, senior product manager for the NHS App, explained why the NHS App team want to open up the app to more suppliers offering online consultation services and welcomes the latest service to integrate.
- Rupesh Thakkar, implementation lead at NHS England, described how the repeat prescriptions feature on the NHS App impacted primary care services in his area.
- NHS England reported that the number of repeat prescriptions ordered via NHS App was up by compared with last year, although the majority of orders made digitally are made using other tools. The group’s pharmacy representatives previously commented that NHS App does yet notify the nominated pharmacy of orders preventing the pharmacy from having an ability to check whether the items ordered have been inadvertently missed from patients’ prescriptions.
- Digital Health reported on Newcastle Hospitals’ patient engagement platform integration with NHS App.
- The i reported that NHS App could allow patients to shop around hospitals for shortest waiting time.
Patient tools
- Community Pharmacy England reported on pharmacy use of patient apps.
- Boots Pharmacy described their approach for expansion of patient digital tools.
- NHS Digital explored using content types to transform the NHS website.
- NHS Digital announced that online GP registrations reached 240,000 as the new digital NHS service grows.
- Open Access Government reported on adopting a digital-first public sector service approach.
- The NHS Covid-19 app is to be discontinued on 27 April 2023 following a steady decline in the number of active users.
- Digital Health strategist Lia Ali discussed how bringing user-centricity into health innovation improves patient outcomes.
- BBC reported on the tech helping women manage the menopause.
- Medical Futurist reported on the landscape of skin-checking apps.
- The HearO smartphone app is in clinical trials to assess how it can predict heart failure deterioration using AI technology.
- Eight new NHS online therapy courses and apps were conditionally recommended by NICE to help treat depression.
- Imperial College London reported that a genetic test already used routinely in the NHS can guide the use of chemotherapy in people with bowel cancer, new research has shown.
- NICE backed digital therapies for depression within draft guidance.
- Northumbria University reported that Wearable device provided support for Parkinson’s patients.
- Organisation for the Review of Care and Health Apps (ORCHA) chief executive officer explained why digital health is essential to relieve pressure on urgent care.
- An evaluation was conducted of the myDiabetes tool, and findings drawn about whether such apps can improve education and ongoing self-management of healthcare. The summary findings of this study were that “there is potential for increasing diabetes education rates by offering patients a digital option in combination with traditional service delivery which should be substantiated through future research.”
Digital inclusion
- King’s Fund published: Ensuring digitally enabled health care is equitable and effective for all.
- The Department for Work and Pensions plans to make its digital services more accessible and improve data-sharing with the NHS as part of a range of reforms intended to improve disabled people’s experience of the benefits systems.
- Kingston University student helped launch UK’s first tech-led LGBTQ+ sexual health service.
Electronic health records usage
Direct Care APIs and GP Connect Update/Access Record
GP Connect enables GPs and other authorised health care organisations to link in with GP system information, allowing those authorised to use additional access/update record functionalities. NHS England’s Transformation Directorate have updated the GP Connect further since the last workstream update.
The Direct Care APIs programme creates and manages multiple NHS IT products including the GP Connect products. The GP Connect products allow information to flow across health and care systems and geographical boundaries in a structured way in support of direct patient care. The vision of the Direct Care APIs programme is to provide a single mechanism to share information across health and care systems and across boundaries in support of direct patient care.
These are a mixture of GP Connect products:
- Access Record HTML: A read only view of the patient’s record held by the GP practice, including free text and coded entries but excluding documents and attachments.
- Access Record Structured: The patient’s full record held by the GP practice, in structured coded format which can be ingested and saved into the consumer record.
- Send Document: Send a PDF document from one care setting back to the registered GP Practice.
- Update Record: Send structured coded information back to the registered GP Practice to allow auto-ingestion of that information.
- Appointment Management: Book, amend and cancel appointments in a primary care setting.
- Patient Facing Services: supporting replacement of legacy technology to provide structured data into the PFS to drive ‘Mobile First’ citizen behaviour.
‘Access Record Structured’ and community pharmacy: In order to improve community pharmacy access to information, the development of Access Record will allow pharmacy staff to view patient information in their local systems. All GP system suppliers are either ready to proceed with first-of-type piloting or are currently in the ‘assurance stage’ (which is progressing well). NHS England would like to work with community pharmacy suppliers to ingest a tailored dataset from the GP to support the patient consultations of pharmacies.
‘Update Record’ and community pharmacy: To improve the flow of data from community pharmacy to GP Update Record will allow information relating to Medications dispensed, Observations taken and a summary of the encounter to be sent back to the registered GP and will be auto-ingested. The next time the patient record is viewed, the information from community pharmacy will be available as part of the ongoing patient GP record. Observations will also be made available via PFS solutions alongside observations taken at the GP Practice to support presentation of holistic patient observations. Technical specification is currently being reviewed by GP suppliers and will be shared with community pharmacy after this session.
Electronic health records usage within community pharmacy
- Community Pharmacy England reported on the Summary Care Record application portal being replaced by National Care Records Service.
- Shared Care Records (ShCR) are patients’ electronic health records. ShCRs include information from multiple care settings, e.g. GP practice and secondary care. Most English patients live within an area with a records project ongoing. Shared care records are emerging across the country and the IT has been maturing, with the aim being that over time more health and care professionals can access these records. LPCs and/or local pharmacy members can continue to take steps to gain pharmacy access and should use the guidance set out in the ‘Engagement’ section of Community Pharmacy England’s community pharmacy and ShCRs webpage.
- Community Pharmacy England has been encouraging pharmacy IT support to ensure that ShCR, NCRS and records links are authorised for use via communications with the CP ITG whitelisting mailing list.
- Community Pharmacy England continues to work with NHS England’s Transformation Directorate and other relevant stakeholders on the actions set out within the Shared Care Record (ShCR/LHCR) NHS Transformation Directorate and pharmacy outputs and actions LPCs, ShCR project teams and other parties supporting ShCR pharmacy deployment are encouraged to contact it@cpe.org.uk with any technical ShCR information so that supplier and IT support helpdesks can authorize multiple ShCR domains simultaneously.
Records: national
- Oracle Cerner’s vice president opined that the NHS should not treat the implementation of electronic patient records as IT projects and instead view them as a “transformation process improvement”.
- Digital Health published a special report on Usability and why secondary care electronic patient records systems (EPRs) can and should do more.
- HSJ reported that although electronic patient records are regarded as an essential to delivering better care, there is evidence that records systems without optimal usability may contribute towards clinician burnout.
- The GP Connect team conducted user research on the GP Connect Structured FHIR API solution, and CP ITG suppliers were encouraged to consider participating.
Records: local
- The Greater Manchester Care Record (GMCR) ShCR project team hosted a community pharmacy IT supplier kick-off meeting on 19th April 2023 and many of you will have attended. It set out potential integration work and the advantages for supplier s considering this – including funding contributing towards development. This webinar had explained:
- their records project and the footprint of nearly 700 pharmacies;
- direct award incentive funding offer to support pharmacy IT supplier development;
- ability for suppliers to develop Single-Sign-On and One-Click; and
- learning for future ShCR and NHS records interoperability work.
- The GMCR team were made aware that CP ITG reps including suppliers reps had fed back that improvements were needed to be made to underlying coding and protocols including NHS IT standards (so that fewer different integrations would be required for suppliers to plug into multiple NHS records systems).
- Saint Catherine’s hospice became the first to use the Yorkshire and Humber Shared Care Record.
- Mid and South Essex Integrated Care System commissioned the Patients Know Best platform for its patients, to support access to personal health care records.
- NHS Western Isles Health Board expanded its use of Cambric Systems’ Morse Electronic Patient Records app, which aimed to enable more joined up patient care within Scotland.
- Patients Know Best supplied more NHS trusts with personal health record solutions.
Genomics
- Source BioScience has opened a new Genomics and Precision Medicine Centre in Cambridge.
- CNN reported that 100,000 new-born babies will have their genomes sequenced in the UK -potentially with implications that may develop how child medicines are prescribed and dispensed in the future.
- BMJ published an article on genomics and patient expectations surrounding genetic risk factors.
Other records updates
- SCR AI changes continued beyond COVID-19 legislation which expired during 2022. Community Pharmacy England and the Community Pharmacy IT Group have campaigned for pharmacy teams’ access to SCR AI to be extended beyond the pandemic by sharing case study information. If you have any examples of how SCR with AI has enhanced patient care, in comparison to normal SCR access, please contact it@cpe.org.uk, as such examples could be used to support the case for permanent access to SCR with AI and other health records for pharmacy.
Standards and interoperability
- At a previous meeting, the group agreed to support the capability for anonymised data to be accessible, so that pharmacy teams’ interventions can start to be auditable, and the value of community pharmacy can be better demonstrated. If PMR systems were to be adapted to allow such data sharing, it would require the development of a roadmap and a standard approach to data provision, which may benefit from use of SNOMED CT clinical terms. If you would like to help with this work, please contact it@cpe.org.uk.
Straightforward security & connectivity
Data Security and Protection Toolkit (DSPTK)
- Community Pharmacy England updated its Data security and information governance hub and published new guidance documents for the 2022/23 Toolkit submission. Additionally, Community Pharmacy England and the NHS DSPTK team jointly presented a webinar on the topic, which around five hundred people registered to attend. The new DSPTK webinar was subsequently made available on demand. Community Pharmacy England and the NHS DSPTK team are working on the arrangements for the community pharmacy 2023/24 toolkit publication ahead of the next June 2024 deadline. If you would like to feed into the development of the 2023/24 toolkit, please email it@cpe.org.uk.
NHS IT services & older browsers
- Previous bulletins have provided updates regarding NHS IT becoming non-compatible with older versions of Internet Explorer (e.g. 7, 8, 9 or 10). NHS England’s Transformation Directorate security team have said that using unsupported browsers and systems makes organisations vulnerable to cyber security threats and performance may also be impacted. The Transformation Directorate have been communicating that some NHS IT services will no longer be compatible with Internet Explorer version 7, 8, 9 or 10 from 22nd June 2023. This may include NHS Spine application, Patient Demographic Services (PDS), MeshUI, Electronic Prescription Service Prescription Tracker, Spine alerts and Summary Care Record application (SCRa). NHS Credential Management and NHS Identity Agent software is also recommended for Smartcard authentication. Pharmacy IT support and Patient Medical Record suppliers may have assisted with system setup to include such software on managed terminals. NHS statistics suggest almost all pharmacies have already migrated onto newer browsers, but if there are any remaining pharmacy organisation (large pharmacy organisations as well as smaller ones) who have not done so yet, then migration plans can be implemented.
NHS Profile Manager
- Previously, community pharmacy teams used two different NHS systems to ensure their pharmacy details were up to date in the Directory of Services (DoS) and on the NHS website: the NHS website profile editor and the DoS Profile Updater. During late 2022, NHS Profile Manager launched to replace both the DoS Updater and the NHS website editor. Newer features within NHS Profile Manager mean you can now:
- update your facilities, e.g. confirmation of facilities such as car parking; and
- confirm whether you provide the NHS blood pressure check service and Pharmacy Contraception Service – within the service module.
- Community Pharmacy England published an NHS Profile Manager Spring 2023 reminder.
Next steps:
- NHS England’s Transformation Directorate continues to work with the pharmacy multiples regarding the NHS website and DoS Application programming interface (API).
- If pharmacy representatives wants to discuss the potential enhancements on the wishlist, please contact it@cpe.org.uk.
Other data security updates
- DHSC published a report on Cyber security strategy for health and social care: 2023 to 2030. This report set out how the government plans to achieve cyber resilience across the health care sector no later than 2030. Digital Health reported on this.
- NHS England’s cyber team said that:
- NHS England’s Transformation Directorate (NHS TD) patient safety team blogged that everyone working in health and care should protect the NHS from cyber-attacks, and that clear, supportive messaging will help people do their bit.
- Bennett Institute for Applied Data Science outlined why information governance is not enough when it comes to protecting privacy.
- Netskope Threat Labs has warned that threat actors are increasingly using cloud apps to target healthcare organisations with cloud malware delivery – rising from 38% to 42% in the past 12 months.
- Open Access Government reported that in order to establish an effective digital healthcare system, we need to build trust with privacy first, argues Nigel Jones, co-founder of the Privacy Compliance Hub.
Smartcard identity checking process to be digitized: Apply for Care ID
- Pharmacy team members must authenticate their identities to be linked to their Smartcards. Prior to the pandemic, pharmacy team members had to attend face-to-face meetings with local Registration Authority (RA) staff. The NHS implemented emergency policies throughout the pandemic so that staff could authenticate themselves remotely, e.g., via video calls. NHS England’s Transformation Directorate hopes that a successful early rollout will lead to the wider rollout of ‘Apply for Care ID’. This programme will enable health care staff use an NHS authenticator app as an alternative to a face-to-face visit to the RA. The service has incorporated feedback from Community Pharmacy England and CP ITG into their plans. The ‘Apply for Care ID’ online materials have been further updated since the last pharmacy IT bulletin.
Connectivity
- Digital Health reported that a new generation of 5G connectivity can unlock innovative approaches to treatment.
Policy and general updates
Pharmacy Show: Agenda re pharmacy IT
The Pharmacy Show has been the largest face-to-face gathering of pharmacy professionals during recent years. The next Pharmacy Show is scheduled for 15th-16th October 2023. It will include sessions regarding pharmacy IT.
IT policy: organisational changes and updates
- NHS England has plans to merge data with private healthcare institutions to process and share information on healthcare activity.
- NHS England and Health Education England have legally merged to create a new, single organisation to lead the NHS in England.
- NHS England’s digital chief Tim Ferris to leave in September.
- King’s Fund speakers opined that Digital transformation of the health service will only be successful if innovators feel free to experiment and those who control budgets are realistic about the timeline for change.
- DHSC was seeking a “key senior leader” to advise the health secretary on digital, data and innovation.
IT policy: Delivery plan for recovering access to primary care
- The Government and NHS today promised a £645m investment in community pharmacies over the next two years to support a pharmacy common conditions service, along with the NHS Pharmacy Contraception and NHS Hypertension Case-Finding services. The Delivery plan for recovering access to primary care referenced digital development:
“As part of the new funding and to ensure the highest standard of care for patients, we will invest to significantly improve the digital infrastructure between general practice and community pharmacy. NHS England will work with community pharmacy suppliers and general practice IT suppliers to develop and deliver interoperable digital solutions. These will streamline referrals, provide additional access to relevant clinical information from the GP record, and share structured updates quickly and efficiently following a pharmacy consultation back into the GP patient record. These IT improvements will improve existing and future services; for example, by allowing GP patient records to be updated following supply of oral contraception or a blood pressure consultation in community pharmacy.”
IT policy general updates
- The ‘key to the future of pharmacy IT’ infographic was updated following feedback from CP ITG and pharmacy members. Pharmacy members may provide further feedback to it@cpe.org.uk so that this infographic can be iterated as required.
- Community Pharmacy England published a roundup of Spring pharmacy IT developments.
- Pulse reported that the Government will digitise the NHS Health Check, which it said would ‘identify and prevent more cases of cardiovascular disease’.
- NHS Digital reported on engagement events and activities regarding NHS Spine development.
- HSJ reported that Microsoft’s roundtable of senior digital leaders found four focus areas that can help upscale the automation efforts in the NHS.
- NHS England published a report, Who Does What. This report aims to assist NHS England and integrated care system IT leaders to move forward together, following on from the commitments laid down in DHSC’s 2022 plan for digital health and social care.
- Practice Director of SCC Hyperscale, Damon Crawford, argues that three factors influence the SCC approach to working with NHS organisations on new solutions.
- BT published its annual report, Mind the gap: delivering digitally enabled change to the NHS. The related survey had asked NHS professionals to share their thoughts on digital transformation.
- GE Healthcare Europe shared views on the need for healthcare digitisation. It also outlined potential strategies for achieving digitation.
- Tunstall Healthcare opined on what the future may hold for connected solutions and digital health.
IT policy case studies: social care
- DHSC published guidance that sets out the government’s roadmap for transforming adult social care data in England.
- Digital Health reported on how the Government had been unable to meet its digital commitments to social care.
- PRSB and nursing representative Claire Sutton made the case for standardising digital social care records to help people live well for longer.
- Digital Social Care launched a guide to help Councils and social care providers avoid pitfalls when introducing new and emerging technology.
- County Councils Network published a report on Adopting the right technology to transform social care. The report looks into the impact of digital technology on adult social care, and the importance of implementing digital change across the care landscape.
IT policy case studies: GP and urgent treatment centres
- Dr Shanker Vijay, GP and Digital First Lead for London, explained why he was championing the national ‘Register with a GP surgery’ service and talks about improvements to the service.
- Dan Wintercross, Programme Director GP IT Futures at NHS Digital, explained the benefits of getting involved with the early adopter programme, which is giving GP practices the opportunity to shape the future of digital, data and technology in primary care.
- Digital Health reported that the shares in digital health firm Babylon Health fell sharply on news that the company is to be taken private as part of a new debt plan.
- RCGP published: Fit for the Future: GP Pressures 2023.
- BMJ opined on How can we improve the quality of data collected in general practice?
- Loughborough Urgent Treatment Centre will use the eTriage system from eConsult in a bid to tackle lengthy queues.
IT policy case studies: Secondary care
- NHS England plans to create 3,000 additional ‘virtual ward beds’ this year.
- NHS Digital launched a consultation on sharing data from private hospitals with NHS.
- Health strategist Sarah McGovern said that medication administration incidents have significantly reduced following the go live of an electronic patient record at the largest trust in the UK.
- NHS England is making a dynamic purchasing system its approved procurement route for trusts buying equipment and systems to run virtual wards and remote monitoring programmes.
- NHS Providers published a guide on effectively embedding digital in your trust.
NHS use of big data to support patient care and clinical research
- Boots UK managing director Sebastian James said that innovative data sharing between the NHS and community pharmacy could deliver a huge leap forward in early prevention of disease and improved management of long-term conditions.
- Forbes reported on the NHS Federated Data Platform, which aims to bring all the data handled by the NHS together into a single source where it can be used to improve decision-making and patient outcomes.
- Digital Health published reports on:
- Institute for Government outlined Government data sharing during the pandemic – the benefits and what enabled the change to practices and behaviours.
- Forbes reported on the building of the NHS Federated Data Platform – arguably the world’s largest healthcare data platform.
- The non-profit legal advocacy group Foxglove flagged upcoming challenges with managing procurement and information governance risks during the selection process for the provider of NHS England’s Federated Data Platform (the incumbent was Palantir).
Artificial Intelligence (AI)
- Pharmaceutical Journal reported on datasets of patient data and AI replacing clinical decision support rules.
- Microsoft said that innovative technologies powered by AI can boost NHS productivity and help it recover from the pandemic.
- The Secretary of State for Health and Social Care says the UK government’s investments in AI can help show the value of new technologies while accelerating their use in the NHS.
- The Government launched a white paper on the use of AI, to drive responsible innovation and maintain public trust in this revolutionary technology.
- Medical Futurist reported on a Physician’s visual guide to AI.
- NHS England has launched an AI and digital regulations service for health and social care.
- Mirage reported on a new AI software that can help to spot prostate cancer is being trialled by researchers at Oxford University Hospitals NHS Foundation Trust.
- NHS England pilots AI software to cut missed hospital appointments.
- University of Manchester reported that AI and Digital Healthcare Technologies Capability framework published.
- The Health Foundation considered the opportunities and ramifications for AI use within health care.
- NHS England Transformation Directorate’s Director of AI said AI regulatory framework and workforce training are key AI priorities.
- Tech Monitor reported that many governments are reconsidering the effectiveness of their national AI strategies in light of recent strides in advancements amongst a string of AI technologies.
- NetApp’s Head of AI highlighted how beneficial the use of AI can be as a powerhouse tool of transformation in the health care industry.
- Digital Heath reported that AI-driven predictive analytics can help the heaviest users of health services to self-care and save the NHS from disaster.
- Information Age reported that OpenAI, the developer of ChatGPT, has enlisted UK start-up Faculty to help businesses generate new value opportunities with generative AI.
- A new regional NHS programme is using AI technology to identify high-risk patients on waiting lists to help reduce their risk of deterioration.
IT policy: priorities, reports and the future
- Global Legal Group published a report: Digital health laws and regulations: emerging trends in the global regulation of digital health – 2023.
IT policy (local): Integrated Care Systems
- The Rt Hon Patricia Hewitt was commissioned to lead an independent review of integrated care systems in November 2022. The report was published in spring 2023: The Hewitt Review: an independent review of integrated care systems. Members of the health tech industry shared views on Patricia Hewitt’s review of ICSs.
- More than half of ICSs reportedly lacked ‘crucial’ health management systems.
- West Country ICS introduced new ‘intelligent care traffic control centres’, using AI technology intended to visualise current healthcare demand, capacity and to predict future need.
- NHS Confederation reported on Tom Loosemore and Deborah El-Sayed exploring how integrated care boards can capitalise on the digital revolution.
- Bedfordshire, Luton and Milton Keynes Integrated Care Board has rolled out new technology across its websites to help make information about health and care services easier to access.
- DrDoctor, the patient engagement solution secured £10 million of investment to advance its plans for delivering patient-initiated models of care to integrated care systems.
- HSJ reported on their recent Digital Transformation Summit, where board representatives from ICS and provider organisations discussed the most pressing issues confronting digital health leaders.
- East of England Ambulance Service NHS Trust is to become the first ambulance service to pilot new technology that provides robust connectivity for ambulance crews and vehicles, even in areas where cellular connectivity is impossible.
Digital inclusion
- Electronic Immigration Network reported on how digital exclusion negatively impacts the health and well-being of asylum seekers.
- National Voices published a report on Tackling inequality and disadvantage: Key actions policy makers, commissioners and provider organisations can take when developing an approach with a digital component.
- The King’s Fund explored moving from exclusion to inclusion in digital health and care.
Innovation
Digital capabilities
- Health Education England (HEE) conducted a review looking at the progress made on recommendations from the 2019 Topol Review.
- A BT study found that nearly three-quarters of NHS staff believe technology could help transform patient care in England, with more than 80 per cent claiming it could attract more ’digital natives’ into the workforce.
- TechHQ reported on the uptake of digital technology within the health care sector.
- A research project finds connections within secondary care of connection between digital maturity and patient safety ratings.
- Imprivata launched two free tools: the Digital Identity Maturity Model and Digital Identity Maturity Assessment.
- Claire Read reported that NHS England’s new digital maturity assessment questionnaire can support valuable discussions about local priorities, one of those involved in the pilot has said.
- Digital Health Academy added a new foundation-level module that aims to bridge the engagement gap between health innovators and patients.
- BMC Medical Education published a study: Evaluation of the impact of technical physicians on improving individual patient care with technology.
- BCS Echo reported that pharmacists at Basildon Hospital were among the first to be trained using bespoke virtual reality technology.
Technology
- PocDoc expanded across Community Pharmacy (across 300 locations and four large community pharmacy chains ), powering digital Health Checks.
- NHS Digital described plans to modernise the NHS Spine platform and invited IT professionals to help shape its future.
- Consultant Connect opined that effective digital triaging and consultation programs hold the promise of shifting pressures from overburdened parts of the NHS such as general practice and A&E.
- NHS England Transformation Directorate’s cloud team said more NHS organisations should migrate to the cloud and explained the help available.
- The Chancellor of the Exchequer’s ‘budget for growth’ has laid out the UK government’s proposed road to making the country a ‘science superpower’. Over five years, £310m will be provided to continue facilitating digital health innovations for mental health, musculoskeletal and cardiovascular conditions. The implementation of such digital technologies is intended to alleviate pressures within the NHS.
- Medical Device Network reported that following news of proposed rule changes that will allow greater controlled-medication flexibility, telemedicine’s usage is reaching beyond the original pandemic-related framework.
- Sheffield University researchers found remote technologies help occupational therapists get patients home quicker.
- UK Parliament published a research briefing on medical technology regulations and the NHS.
- Tech Explore reported on Garmi a product of a new sector called geriatronics, a discipline that taps advanced technologies like robotics, IT and 3D technology for geriatrics, gerontology and nursing.
- Partner at global intellectual property firm Marks & Clerk, discussed the importance of medical technology and how efficiencies could be improved within the health sector.
- Med Tech reported on 3D printing within healthcare.
- Diginomica opined whether the Metaverse can be fit for purpose for optimal healthcare services?
- University of Cambridge researchers found that robots can help improve mental well-being at work—as long as they look right.
- MedTech reported on its FUTURES Conference which highlighted NHS’s need for technological solutions.
Culture
- The King’s Fund explored how Tech transformation disrupts leadership styles.
- NHS England’s digital workforce strategy team said that success for NHS is when the organisation is not using the word ‘digital’ and it instead becomes “a fundamental part of our DNA”.
- NHS Providers published new summary guidance on what makes a digital transformation a success. Digital Health reported on this.
Interoperability
- PRSB’s chief executive officer said that healthcare professionals are working flat out to provide care – which makes it the ‘perfect’ time to digitally transform services.
- Product Owner of the NHS API Developer Community, talked about how they’ve improved support for teams integrating with their products and services – and outlines their next steps.
- Hazel Jones from Made Tech discussed how to improve the adoption of open source in the NHS?
Seamless referrals & appointments
Booking and Referral Standards (BaRS) update
NHS England’s Transformation Directorate’s BaRS programme aims to enable booking and referral information to be sent between NHS service providers in a format useful to clinicians. The intention is that BaRS will eventually be available in all care settings. CP ITG feedback indicated that the BaRS programme should be expanded to incorporate NHS appointments standards.
Referrals & appointments updates
- Following the deployment of a specialist outpatient scheduling system, Leeds Children’s Hospital has delivered more than 1,700 additional outpatient department clinics.
- NHS England launched a campaign to encourage all acute trusts to give patients the ability to make appointments and receive messages online.
Optimal principles across all pharmacy IT
- NHS Digital explained why they’ve put sustainability into the NHS digital design principles.
- Kelly Calvert, health strategist explained why supporting efficient workflows is essential in the deployment of medical devices.
IT policy updates
Pharmacy IT priorities: overview
NHS England, DHSC and the CP ITG have previously flagged the pharmacy IT priorities: PRSB Community Pharmacy Data Standard / Community Pharmacy Contractual Framework (CPCF) IT; records access; payment and data APIs; Booking and Referral Standards (BaRS); and EPS next generation. These priorities align with the CP ITG’s vision and the CP ITG’s paper about digital transformation within the NHS. The CP ITG has continued to support these projects and PSNC is also working with the NHS on the next steps to progress these areas. Updates are also expected in relation to:
- Pharmacy IT supplier frameworks: NHS England previously fed back it continued to explore commercial requirements and opportunities that will support both the needs of the sector and system suppliers now and in the future to support and develop an open supplier market.
- Booking and Referral Standards (BaRS): NHS England’s Transformation Directorate’s BaRS programme aims to enable booking and referral information to be sent between NHS service providers in a format useful to clinicians. The intention is that BaRS will eventually be available in all care settings. Pharmacy use cases for the standard are currently being considered – including the potential for referrals from NHS 111 to community pharmacy. The minutes and slides from the group’s previous meeting contain additional information about BaRS. CP ITG feedback indicated that the BaRS programme should be expanded to incorporate NHS appointments standards.
- GP Connect: GP Connect enables GPs and other authorised health care organisations to link in with GP system information, allowing those authorised to use additional functionalities, including “Access Record”. The minutes and slides from the group’s previous meeting contain further information about developments with the GP Connect Access Record.
Independent prescribing
The General Pharmaceutical Council (GPhC) previously consulted and reported on changes to the requirements for entry to independent prescribing courses, and the Pharmaceutical Journal reported that independent prescribing piloting was to begin across England from 2023. NHS England previously reported into the CP ITG about the plans for the pathfinder programme. A special CP ITG meeting was held on 1st December 2022. Each Integrated Care Board (ICB) was invited to complete an expression of interest form working with their Regional Pharmacy Integration Leads and local stakeholders.
Next steps:
Digital priorities
The group has previously discussed pharmacy IT priorities and objectives some of which continues to feed into the CP ITG’s digital vision work. The collated feedback has identified requests relating to the below:
- That referrals always be electronic and align to common NHS IT standards
- That patients can book an appointment with any pharmacy using online methods including through NHS App or pharmacy apps (which should align to BaRS).
- That community pharmacy data flows to and from pharmacy (including expanded Community Pharmacy Data standard).
- That patients be notified digitally about their NHS prescriptions and NHS pharmacy services with standardised messages: e.g. via email, SMS text message, app notification, or online account updates. For example, the EPS prescription statuses ‘ready to be collected’ and ‘delivered’.
- That the Electronic Prescription Service be enhanced in readiness for the next generation.
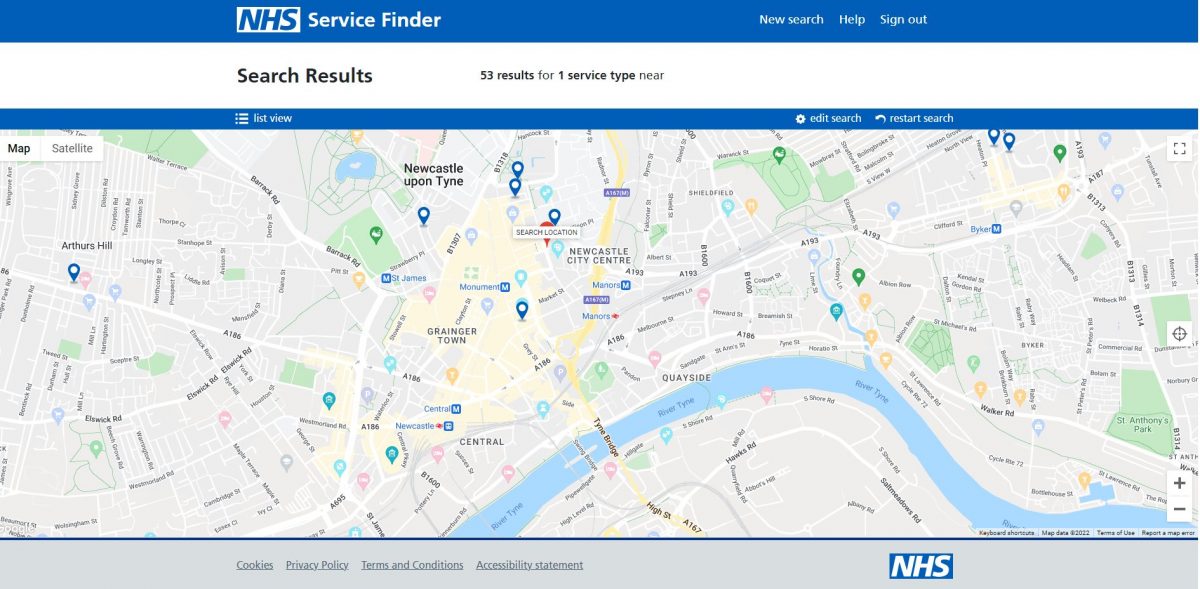
- That patients be able to look-up any service and quickly see which nearby pharmacies offer which services (the Australian pharmacy service finder provides an example model: findapharmacy.com.au).
- Electronic health records usage: Pharmacy requires records and genomics information accessible within its clinical systems with some interim steps expected to be necessary along the way (NCRS and new information made available within this – ShCR portals and information retrieved via GP Connect Access Records etc.).
- That NHS pharmacy services and dispensing elements have IT frameworks and APIs to reduce double data entry. These should be prepared minimum six months prior to service launch.
- That paperless processes be used within community pharmacies.
- That outcomes data is captured and built into pharmacy and dispensing services.
- The Pharmacy IT Futures framework should be established to incentivize innovation and alignment of pharmacy systems to CPCF developments.
- Secure and simple authentication: for pharmacy teams and patients during the delivery of NHS pharmacy services.
Next steps:
- Additional comments about the future development of the infographic can be sent to it@psnc.org.uk.
Payment and data Manage Your Service (MYS) APIs for CPCF services
NHS England and PSNC want suppliers to be given information about the service, including the IT implications and dataset requirements. Progress in this area will reduce the administrative burden and data entry for pharmacy teams, meaning they will not need to copy and paste across different systems. NHS England are encouraging related developments to be accelerated. NHSBSA continue to develop further API specifications for suppliers to align to. The MYS APIs to be prioritised will be Pharmacy Contraception Service, Discharge Medicine Service, Blood Pressure Checking Service, New Medicines Service and the Smoking Cessation Service.
dm+d medicine code changes
Paul Wright and Kerry Frenz (NHS England’s Transformation Directorate) previously engaged with CP ITG suppliers and other stakeholders regarding dm+d code changes. These included the need to shift to use of UK extension identifiers for all virtual medicinal product (VMP) concepts required to enable adaptation dm+d because of global changes to SNOMED CT terminology. Two CP ITG supplier meetings were held: an introductory webinar on 12th October 2022 (which was also made available for suppliers on-demand) and a check-in meeting on 15th February 2023. Paul Wright and Kerry Frenz likewise offered supplier one-to-ones to support the changes. The guidance for suppliers has been updated. Suppliers are encouraged to share comments and feedback by completing the new supplier dm+d code change snap survey and/or by emailing it to it@psnc.org.uk.
National Care Records Service (NCRS)
The National Care Records Service (NCRS) is being introduced as a new interface available from within the Spine portal link directory to provide national patient information for health and care staff. NCRS will be a successor to the Summary Care Record application (SCRa) portal. NCRS enables view of SCR information as well as:
- Personal Demographics Service;
- National Record Locator to locally held care plans
- Reasonable Adjustments Flag
- Child Protection Information Sharing
Information within NCRS is consumable by IT system suppliers. Authorised health and care workers can access the NCRS using mobile or desktop devices connected to the internet using WiFi, mobile data or an existing Health and Social Care Network (HSCN). The NCRS offers multiple access options including biometric authentication or smartcards. The NCRS was piloted within different health and care settings including within Weldricks pharmacies. It is now being rolled out further following the success of the pilots. CP ITG feedback has requested for ShCR pointers, ShCR information, and GP Connect information to be added to the NCRS portal in due course (as an interim given that ShCR information is not yet embedded into clinical systems). Pharmacy teams have also called for the underlying IT standards to unite NCRS and ShCRs so that suppliers which integrate into NHS records systems may easily integrate into any others.
Next steps:
- Pharmacy professionals are encouraged to test out NCRS by going to: https://portal.spineservices.nhs.uk/nationalcarerecordsservice/ (on their Patient Medical Record (PMR) machines with their Smartcard) and completing this NCRS feedback snap survey (or email it@psnc.org.uk) to confirm if you can access it and your experience of using it.
Appointments systems
The group previously considered the management of appointments using IT systems. Past feedback from the group is below:
- Integration is required across appointment systems.
- Avoidance of the management of multi appointment systems.
- Patients should receive sight of appointments information.
- The BaRS programme should incorporate appointment standards.
- Appointment systems should seek to reduce the login burden.
The NHS website team have asked for feedback about pharmacy team use of appointment systems.
Next steps:
Interoperability and records
NHS Profile Manager
- Previously, community pharmacy teams used two different NHS systems to ensure their pharmacy details were up to date in the Directory of Services (DoS) and on the NHS website: the NHS website profile editor and the DoS Profile Updater. During June 2022, NHS Profile Manager launched to replace both the DoS Updater and the NHS website editor2. The services module was launched during late 2022 and further service module enhancements are anticipated this year. Since mid-January 2023, pharmacy teams have been able to update NHS Profile Manager if they routinely hold the 16 palliative and end of life care (PEoLC) medicines listed in the Drug Tariff and can support local access to parenteral haloperidol.
- A series of NHS Profile Manager video tutorials from NHS England are available to support pharmacy teams to use the tool.
- PSNC published a news item about how all community pharmacy Directory of Service (DoS) and NHS website profiles were automatically set to show as closed on Christmas Day (although this could be changed by the pharmacy team – if required).
Next steps:
- NHS England’s Transformation Directorate continues to work with the pharmacy multiples regarding the NHS website and DoS Application programming interface (API).
- If the group wants to discuss the potential enhancements on the wishlist, please contact it@psnc.org.uk.
Electronic health records usage within community pharmacy
- Shared Care Records (ShCR) are patients’ electronic health records. ShCRs include information from multiple care settings, e.g. GP practice and secondary care. Most English patients live within an area with a records project ongoing. Shared care records are emerging across the country and the IT has been maturing, with the aim being that over time more health and care professionals can access these records. LPCs and/or local contractors can continue to take steps to gain pharmacy access and should use the guidance set out in the ‘Engagement’ section of PSNC’s community pharmacy and ShCRs webpage.
- PSNC has been encouraging pharmacy IT support to ensure that ShCR, NCRS and records links are authorised for use via communications with the CP ITG whitelisting mailing list.
- PSNC continues to work with NHS England’s Transformation Directorate and other relevant stakeholders on the actions set out within the Shared Care Record (ShCR/LHCR) NHS Transformation Directorate and pharmacy outputs and actions documents. LPCs, ShCR project teams and other parties supporting ShCR pharmacy deployment are encouraged to contact it@psnc.org.uk with any technical ShCR information so that supplier and IT support helpdesks can authorize multiple ShCR domains simultaneously.
- A pharmacy ShCR progress table sets out some of the activity.
- CP ITG participants took part in NHS England’s NCRS introductory webinar events held on 2nd February 2023 and 7th February 2023.
PSNC, CP ITG and NHS England’s Transformation Directorate jointly ran an event to progress the records agenda on 8th December 2022 (see papers and slides). Some of the feedback from this event is replicated below:
- The goal is for structured clinical information to be directly accessible within clinical systems – following the development of structured coding which sits under NHS records systems.
- The development of underlying IT standards is needed so that a supplier can use NHS APIs so that if the supplier ‘plugs into’ any NHS records system or ShCR system, they will be able to plug into any other easily.
- Common standards are needed for IG and tech relating to ShCR other records.
- More information within National Care Records Service (NCRS) portal would be helpful including ShCR pointers (e.g. links and ShCR one-click), and information accessible via GP Connect – Access Records, and National Record Locator (NRL).
Use of records within GP practice
- Pulse reported on the large budget cut which put into question the rollout of mass GP data extraction, aimed to be shared for planning and research purposes.
- PublicTechnology.net reported on how the NHS launched a new multimillion-pound framework to support the creation and delivery of web-based GP IT systems. Eight suppliers have been awarded a place on the framework: EMIS Health; Eva Health Technologies; The Flame Lily Healthcare; MedicalDirector; JWPM; Medicus Health; Ouris Health; and OX.DH. These suppliers are expected to work with the NHS during 2023-2024 to “develop new GP clinical systems in line” with the standards and required functionality. UKAuthority.com also reported on this.
- Pulse reported technical and operational challenges with the ‘Citizen’s Access Programme’ (this gives patients automatic access to their records through the NHS App).
Other records updates
- SCR AI changes continued beyond COVID-19 legislation which expired during 2022. PSNC and the Community Pharmacy IT Group have campaigned for pharmacy teams’ access to SCR AI to be extended beyond the pandemic by sharing case study information. If you have any examples of how SCR with AI has enhanced patient care, in comparison to normal SCR access, please contact it@psnc.org.uk, as such examples could be used to support the case for permanent access to SCR with AI and other health records for pharmacy.
- DigitalHealth.net published a special report on ShCR progress and positive developments for mature ShCR and ‘skyrocketing progress’ for some of the ShCR projects which were ‘late arrivals’.
- London North West University Healthcare NHS Trust (LNWH) says LNWH has become an entirely paperless Trust after a two-year project which digitised 210,000 patient records.
- TPP boss Hester questioned whether the NHS was receiving value for hospital EPR costs and proposed TPP support.
- The use of the NHS Covid database has been revived with the intention of fighting other diseases.
- DigitalHealth.net reports on the government’s digital agenda regarding the new, Federated Data Platform (FDP). The FDP is intended to bring together siloed data from the 42 Integrated Care Systems to support joined-up health services.
- PublicTechnology.net reported on the government’s plan to invest millions of pounds into supporting digitisation for the half of social-care providers across the country that were still entirely reliant on paper care records.
- The Care and Health Information Exchange (CHIE) ShCR, has been extended into care homes within Hampshire and the Isle of Wight.
Community Pharmacy Data Standard (CPDS)
- PRSB reported previously that it was looking to update to CPDS. This was to reflect changes to the community pharmacy contractual framework in England and the services it covers, along with other changes to bring the standard up to date with, for example, improvements to the underlying sections used in other PRSB standards. The changes to the standard are not altering or bringing in significant new areas of clinical/professional content.
- PRSB arranged two webinars: a supplier meeting (2nd February 2023), and a general webinar (7th February 2023). CP ITG participants were encouraged to attend these. The proposed uplifts are set out within this slide-set. Comments to PSNC can be sent to it@psnc.org.uk.
Standards and interoperability
- The King’s Fund held an event on, ‘Digital technologies and interoperability: enabling the future of integrated care’ and made videos from the event available on-demand.
- At a previous meeting, the group agreed to support the capability for anonymised data to be accessible, so that pharmacy teams’ interventions can start to be auditable, and the value of community pharmacy can be better demonstrated. If PMR systems were to be adapted to allow such data sharing, it would require the development of a roadmap and a standard approach to data provision, which may benefit from use of SNOMED CT clinical terms. If you would like to help with this work, please contact it@psnc.org.uk.
National Booking Service (NBS) ‘proof of concept’ testing of flu vaccination appointment booking
- The NBS, is a digital tool which enables patients to use the internet to book their NHS COVID-19 vaccination appointment.
- NHS England’ NBS team began a ‘proof of concept’ test to consider extending the use of NBS to allow patients to book their flu vaccination appointments through the NBS at pilot pharmacies.
- The CP ITG held a meeting about NBS on 12th October 2022. CP ITG participants fed back that:
- NBS should align to the NHS Booking and Referral Standard (BaRS) at the first possible opportunity, and pharmacy appointment systems should align to BaRS. Development work will be required to enable this to happen.
- If all pharmacy and NHS appointment systems integrated into BaRS this would be expected to lessen the challenge with pharmacy teams needing to manage the burden of multi calendars. Dedicated vaccine appointment systems will help with staff rotas and planning; stock orders; management for just in time deliveries; and patient communications.
- The NBS team said that NBS does not yet integrate into pharmacy appointment systems or BaRS. However, the NHS England NBS team has started discussions with the BaRS team, although integration work has not yet been commissioned.
- The evaluation of the NBS flu ‘proof of concept’ will be conducted during 2022-2023.
- PSNC shared feedback into the NBS evaluation process – which included the feedback from CP ITG participants.
Referrals IT
- A special CP ITG event was held on 25th October 2022. A CP ITG sub-group discussed referrals with the BaRS team, who are generating research to improve the NHS e-Referral Service and the NHS future referrals team (see slides and minutes). The sub-group provided feedback about the current IT used for referrals and about what was needed in the future.
NHSmail
- The NHSmail escalation process and the associated factsheet has been amended. Pharmacy NHSmail users with technical queries about NHSmail are now advised to contact helpdesk@nhs.net instead of pharmacyadmin@nhs.net. The NHSmail team have said this will not change the helpdesk experience. If pharmacy NHSmail users do accidently email the old address pharmacyadmin@nhs.net such emails will automatically be diverted to the helpdesk inbox.
- The NHSmail team made changes to the system regarding keeping accounts active from 1st December 2022. Personal NHSmail accounts which are not used for 30 days will be marked inactive and inactive accounts which are not activated within the following 30 days will be deleted. If a personal NHSmail account is ‘deleted’; it can be restored within 30 days by raising an NHSmail ticket. If an account is not restored within that period, it will be permanently deleted, and it will not be able to be restored.
- The Virtual Visits tool provides pharmacy contractors with an appointments system so that they can notify patients and better manage appointments. Pharmacy teams can also use the Virtual Visits tool to conduct face to face or virtual patient consultations (audio or video).
- The Virtual Visits tool works in conjunction with NHSmail Microsoft Teams and the Microsoft Booking platform. To participate in the pilot, you must have an active personal NHSmail account, access to a shared NHSmail inbox, MS Teams installed on a computer or tablet and a computer or device with a webcam. Contractors that have not done so should register interest with taking part in the Virtual Visits pilot via this webform.
IG, identity and security
Data Security and Protection Toolkit (DSPTK)
- PSNC updated its Data security and information governance hub and published new guidance documents for the 2022/23 Toolkit submission. Additionally, PSNC and the NHS DSPTK team jointly presented a webinar on the topic, which around five hundred people registered to attend. The new DSPTK webinar was subsequently made available on demand. PSNC and the NHS DSPTK team are working on the arrangements for the community pharmacy 2023/24 toolkit publication ahead of the next June 2023 deadline. If you would like to feed into the development of the 2023/24 toolkit, please email it@psnc.org.uk.
Other data Security updates
- National Data Guardian has advised national policymakers that suppliers must share NHS core values.
- DigitalJournal.com explored the impact of recent and future ransomware attacks on NHS IT.
- Chris Day, Cyber Clinical Informatics Manager with NHS England’s Transformation Directorate, argues that cyber security is more than ‘just an IT issue’ and outlines his role in shaping clinical safety and cyber security strategies.
- The Network and Information Systems (NIS) regulations are expected to be extended to additional critical service providers including the NHS and energy companies. The changes include requiring the services to improve their reporting of cyber incidents to regulators of a wider range of incidents that could signal a high risk even if they do not immediately cause disruption. The new measures will also reportedly give the government the power to amend the NIS Regulations – possibly by making them apply to more organisations.
- HSJ, reported that the government looking for a new cyber security chief for the NHS and Department of Health and Social Care, at a time of heightened risk of cyber attacks against the health service.
- The first four regional Trusted Research Environments (TREs) have been confirmed. These are intended to provide a secure space for NHS data research.
Reducing burden
Paperless processing
- Community Pharmacy IT survey results: 83% of pharmacies support going paperless.
- Simon Duncan, the Director of B2B Solutions at E.ON, outlines the key considerations for decarbonising the NHS and the public sector.
Smartcard identity checking process to be digitized: Apply for Care ID
- Pharmacy team members must authenticate their identities to be linked to their Smartcards. Prior to the pandemic, pharmacy team members had to attend face-to-face meetings with local Registration Authority (RA) staff. The NHS implemented emergency policies throughout the pandemic so that staff could authenticate themselves remotely, e.g., via video calls. NHS England’s Transformation Directorate hopes that a successful early rollout will lead to the wider rollout of ‘Apply for Care ID’. This programme will enable health care staff use an NHS authenticator app as an alternative to a face-to-face visit to the RA. The service has incorporated feedback from PSNC and CP ITG into their plans. The minutes and slides from the group’s previous meeting set out additional developments about Apply for Care ID. The ‘Apply for Care ID’ online materials have been further updated during late 2022.
Other updates about reducing burden
- Nuance published a report demonstrating the burden of clinical documentation.
- Building the Future for GP practices report from BMA suggested doctors are losing 13 million hours annually because of NHS IT challenges.
- Graphite’s user research team explained the difficulty of demonstrating the value of health IT user research in health and care.
- Academia Ltd reported on the benefits with mobile tablet usage within health and care.
Development of pharmacy systems
Recommended minimum transfer dataset for pharmacies switching from one patient medication record (PMR) system to another
PSNC previously supported developing a recommended minimum dataset for cases where a pharmacy contractor has switched from one PMR system to another. For the sake of continuity of patient care, it is critical for some patient information to be transferred from the old to the new system. A dataset is being developed incorporating the comments from previous group meetings and suppliers. An associated specification document is also being developed. The working group is to meet again once the dataset is further developed.
EPS and RTEC
Electronic Prescription Service (EPS)
- Pharmacy teams are encouraged to complete the EPS Paperless, Outcomes and Trackability survey (5- 7 mins). The results will feed into a study by Kinston University and will also be shared to the NHS England EPS team.
- The EPS user research team at NHS England are continuing to explore looking at enhancing features within the NHS App, with one potential feature being to provide patients with access to an electronic prescription token or Phase 4 non-nominated token. Pharmacy teams are encouraged to provide feedback via the EPS team survey on digital tokens (past CP ITG feedback on digital tokens passed to the EPS team is set out here).
- It is now 18 years since the first electronic prescription was received by a community pharmacy in February 2005. Back then, the Co-op pharmacy on Scott Street in Keighley, West Yorkshire, received a prescription for atenolol from their local GP practice. Instead of coming into the pharmacy through the front door in the form of a green paper slip in the hands of a patient, the prescription had been sent directly from the GP practice IT system to the pharmacy’s system. It took more than ten years for the transition to be made from paper to digital prescriptions in primary care, as more GP practices added EPS and additional changes were introduced. NHS England’s Transformation Directorate published a feature about the early days of EPS and how it has transformed primary care prescribing in England. PSNC also highlighted the milestone.
- DigitalHealth.net reported on Electronic Prescription Service fulfilling one billion items a year.
- PSNC reported on an additional opportunity to Help improve the Electronic Prescription Service.
- PSNC published a new EPS token ordering and escalation briefing factsheet.
Real Time Exemption Checking (RTEC)
- The NHSBSA continues to lead the RTEC project. The NHSBSA, DWP and the RTEC steering group plan has supported the expansion of the DWP RTEC functionality to additional pharmacy contractors. Over 80% of pharmacy organisations have now received the Department for Work and Pensions (DWP) functionality for Real Time Exemption Checking (RTEC). The group may suggest items for the RTEC development roadmap by emailing it@psnc.org.uk.
Apps, wearables and technologies (incl videocon)
NHS App future developments
The NHS App team are continuing to develop existing and future features including:
Booking or managing a vaccination – Eligible people can now book or manage their COVID-19 vaccine using the NHS App as the National Booking Service has been added to the NHS App. In the coming months, eligible people will be able to book a flu jab on the NHS App.
- Personal Health Records integration with the NHS App.
- Notifications and messages direct to the NHS App: Following a pilot in 2022, NHS App now allows patients to receive messages relating to their care through the NHS App. The NHS App only allows messages from verified health and care services, so patients who are using the service know they can trust the authenticity of every message they receive. Patients need to have enabled notifications for the NHS App to use this feature. The current messages relate to:
- reminders for referral appointments;
- reminders for online consultations; and
- vaccination invitations.
- Hospital appointments: patients are being given more control over their hospital appointments and how and when they access information and support – via NHS App. 23 trusts have gone live.
- Register with a GP surgery: The NHS has introduced an online service to make it quicker and easier for people to register with a new GP surgery, offered free to all GP services. This new service is now being used at over 600 GP practices in England and is available for all GP practices to use.
- Usability improvements: A new introductory ‘carousel’ has been launched and is visible to people using the app for the first time. It describes what the app can do for them.
- Access to GP health records. Since late 2022, patients with online accounts such as through the NHS App will be able to read new entries in their health record. This applies to patients whose practices use the TPP and EMIS systems.
- Test results: NHS App team are currently undertaking discovery work to understand more about the difficulties and pain points patients and clinicians face when it comes to accessing and understanding test results. It is hoped the findings will help NHS App team to prioritise the improvements which will have the most value for patients and clinicians.
Other NHS account and NHS App changes
- The NHS account team provided updates about the changes made to the NHS account See: NHS account release notes.
- NHS website was visited more than 1.2 billion times within a year. DigitalHealth.net reported that NHS website gets 23 million visits per week and 2,300 views per minute.
- Patients can now update their address using the NHS App.
- The government announced that NHS App had topped 30 million sign-ups by the end of 2022. The BBC also reported on this large NHS App usage.
Patient apps, tools and regulation
- DHSC announced a £20 million research fund for developing new medicines and digital tools which demonstrate they will help people shed 20% of their weight.
- CEO of GetUBetter, discussed why digital self-management for people with musculoskeletal conditions or pelvic health problems is finally becoming a reality.
- Mental health funding of £1.8m welcomed by NICE and MHRA to explore regulation of digital mental health tools.
- An expert on medical technology policy discussed the growing popularity of digital mental health tools and the moves to improve their regulation and guidance in the UK.
- Digital mental health technology was recommended for children and young people by NICE.
- The Medicines and Healthcare products Regulatory Agency (MHRA) has received £1m from BEIS’ Regulators’ Pioneer Fund for three projects. The three projects aim to improve how patients access life-changing treatments in clinical trials and to find a way to introduce complex artificial intelligence safely into front-line clinical settings.
- PharmaPhorum.com reported that Wellcome funds were supporting the new regulation of digital mental health tools.
- HTN reported on the development of the ShinyMind health and wellbeing app and positive assessments from Care Quality Commission, and the Academic Health Science Networks.
- MedTechNews.com reported on the emerging ‘Internet of Bodies’ technology and how the integration of Internet of Things (IoT) technologies and medical care has led to a surge in patent applications for connected medical devices. The article also explored trends in wearable and other tracking devices that detect an individual’s vital signs or changes in physiological responses.
- AccuRx integrated its online consultation tool, Patient Triage, with the NHS App.
- BioMed Central (BMC) published a study on NHS Allied Health Professional (AHP) clinicians and whether had sufficient guidance and training for delivery of remote consultations. Most AHP clinicians reported that guidelines had ambiguous areas (e.g., regarding protection from litigation and dealing with emergencies) and that the training that they had experienced was not sufficient.
- NHS Education for Scotland launched a National Digital Platform (NDP) for the building of digital services and apps in health and social care.
Usable IT beyond pharmacy PMR systems and EPS
IT policy: organisational changes and updates
- PSNC reported on how NHS Digital teams and responsibilities were absorbed into NHS England’s Transformation Directorate from 1st February 2023. DigitalHealth.net reported on the changes.
- Legislation which finalised merger of NHS Digital into NHS England aimed to ‘ensure good practice continued – including data protection, transparency and information governance.
- NHS Digital published annual report and accounts 2021 to 2022 during late 2022.
- PublicTechnology.net published an article, NHS Digital said that the 2022 fiscal year, in which £750m was used to advance health IT was likely to be seen as “turning point” in the technological transformation of the health service.
- DHSC reported during late 2022 on how Plans to merge NHS Digital with NHS England were accelerated to early January 2023 to support the ‘plan for patients’.
- Dr Marcus Baw opined that frequent organisational reforms for NHS organisations challenged the ability to make the best progress.
Artificial Intelligence (AI)
- A report published by the NHS AI Lab and Health Education England (HEE) called for all health and care staff to receive training in artificial intelligence (AI).
Parliament’s Health and Social Care Committee inquiry into ‘Digital Transformation in the NHS’
- The Parliamentary Health and Social Care Committee collected evidence during late 2022 relating to changes with digital technology within the NHS. The CP ITG submitted a formal response to Health and Social Care Committee inquiry into ‘Digital Transformation in the NHS’, and additional evidence during late 2022.
- Health and Social Care Committee published its evaluation during February 2023. Its panel rated the government’s progress on digitising the NHS as ‘inadequate’. Its findings included:
“Despite some encouraging progress, the Expert Panel found that key Government commitments on workforce and the use of patient information were either not met or were not on track to be met. The Panel found that overall progress towards improving the digital capabilities of the NHS was too slow, and often lacked support and funding.”
Professor Dame Jane Dacre, the Panel Chair, said:
“What is particularly disappointing is that the Government recognises that the digitisation of the NHS is essential to bring about real benefits to patients, for example by helping them to monitor and manage long-term health conditions independently. Yet time and again, promises have been made but not delivered, hampering wider progress. We heard about issues with interoperability between systems and providers, making it difficult for all parts of the system to communicate effectively, leading to delays and efficiency losses.”
Steve Brine MP, Chair of the Health and Social Committee, said:
“The Panel’s detailed work provides evidence of the Government’s overall ‘inadequate’ approach to its commitments to digitise the NHS and will feed into the Committee’s work, shaping the recommendations we make to Ministers.”
- The full report from the Health and Social Care Committee also noted that:
- The NHS App was is not well integrated with pharmacy which prevents use of the app to manage repeat prescriptions and this may be one of the reasons a very small percentage of repeat prescriptions orders are made using the NHS App.
- The current funding is not sufficient given the scale of the commitment which includes staffing provision as well as technical aspects. Furthermore, funding needs to be ringfenced, sustained and more evenly spread.
- Pharmacy fed back that a lack of common standards hindered interoperability and prevented wider pharmacy onboarding with ShCRs.
- DigitalHealth.net reported on the findings.
IT policy: priorities, reports and the future
- The CP ITG published its Pharmacy IT quarterly round-up after the group’s last meeting.
- The government set out a strategy to increase access to innovative medical technologies. DigitalHealth.net reported on the strategy.
- Pulse reported on NHS efforts which encouraged the public to access GPs via remote consultations, in an NHS advertising campaign intended to reduce pressures.
IT policy (local)
- NHS Providers launched a programme to help leaders of Integrated Care Systems (ICS) advance digital transformation across their locality.
- Tech Monitor provided cybersecurity tips for ICSs.
- Four in five trusts are yet to reach their digitisation targets required by 2025.
- Bolton NHS Foundation Trust has published its digital strategy for 2022-2025, sharing their ambitions to become a digital trust, with focus on digital integration, care, workforce, infrastructure and estate.
Cultural change
- The King’s Fund published a report on ‘Interoperability is more than technology: The role of culture and leadership in joined-up care’.
- DigitalHealth.net published a report which explored the relationships, culture and technology that come with interoperability and opined that “it is no longer discussed as a technology problem, but rather as a complex change that depends upon relationships and culture.”
- The NHS is ‘too static’ and must learn from itself and others said Tim Ferris (NHS England’s director of transformation).
- Flickread.com explored what’s needed for digital interoperability to succeed.
Use of big data within the NHS
- National Data Guardian published a blog which, looked at the upcoming NHS federated data platform and argued that the public’s support for such big data projects is vital to their success.
- The Acute Data Alignment Programme (ADAPt) has been advancing further during 2022-23. This is a joint programme between NHS England’s Transformation Directorate and the Private Healthcare Information Network (PHIN) that is looking to adopt common standards for data collections and performance measures across the NHS and private healthcare. ComputerWeekly.com reported on the development.
- The Institute for Government published a summary of a roundtable discussion with public servants and others on the NHS Covid-19 Data Store and NHS National Data Platform.
- Great Ormond Street Hospital deployed real-time data-sharing with ambulance teams.
- The International Public Policy Observatory published a report considering whether governments had mobilised data correctly and how data could support decision making.
- DHSC reported on Patients having better choice of which GP practice they wished to visit after data showing appointment waiting times was published for the first time.
- A HSJ event considered how data can play a part in addressing long-standing inequities.
Digital inclusion
- The NHS Race and Health Observatory conducted research into the use of digital apps to reduce ethnic health inequalities.
- Preventx explored how technology can be used to define and address inequities in sexual health and improve the health care system.
Innovation
- UK’s first medical drone delivery project (within Scotland) is intended to change future of NHS. The medical drone project is allowing essential medicines, bloods and other medical supplies to be distributed.
- The Crown Commercial Service produced a guide for NHS bodies and trusts carrying out digital transformation: Prepare, Transform, Enhance: Digital transformation in the NHS. HSJ reported on this.
- The Institute of Cancer Research argues that now is the right time for the health care sector to embrace digital innovation.
- MadeTech’s digital transformation team opined how the public sector can improve the efficiency of digital innovation, in order to keep costs low.
Digital capabilities and recruitment
- Seven pharmacy staff from community and hospital settings fed into a study about the digital competencies for pharmacists. The study also assessed Health Education England’s digital capabilities framework tool and found some benefits concerning its usage within pharmacy.
- Health Education England (HEE) reported on how digital technology could improve the performance of the health and care workforce and meet future demand for services. DigitalHealth.net also reported on this.
- The Professional Record Standards Body argued that digitisation is desperately needed in NHS recruitment.
- Pulse reported that PCNs can now recruit 1,000 GP assistants and 1,250 digital transformation leads.
Genomics
- Health Education England (HEE) extended a new online tool for clinicians to help them access vital genomics information for their patients.
IT policy updates
IT policy: organisational changes
- Sajid Javid resigned a week after the digital health and care plan had been published.
- Steve Barclay was appointed Secretary of State for Health and Social Care.
- Mike Potter was appointed as the government’s chief digital officer.
- NHS Digital launched an Innovation Framework for GP IT suppliers.
- Two NHS trusts will end their partnership with health tech company Babylon.
- NHS England chief executive spoke on plans to make the organisation ‘30 to 40 percent smaller’.
Artificial Intelligence (AI)
- Digitalhealth.net reported on AI bias within systems, and how to avoid it.
- An AI expert set out the pros and cons of implementing AI within healthcare.
- Trust in AI among healthcare staff and patients ‘will improve with regulation’ according to a report produced by law firm DAC Beachcroft.
- The Government published a policy paper, Establishing a pro-innovation approach to regulating AI principles for AI regulation.
- HSJ.co.uk reviewed the recent work from the NHS AI lab.
- NHS AI Lab produced a report: Understanding healthcare workers’ confidence in AI.
IT policy: priorities, reports and the future
- NHS Digital signed a deal with Netcompany to deliver improvements to NHS Digital’s Personal Demographic Service. The work involves “several initiatives targeted at increasing the use of NHS number across digital services by making it easier to look up through APIs.
- Research indicates a survey’s respondents views within Trusts indicated that Legacy systems and lack of tech expertise and leadership pose major barriers to NHS transformation.
- American health giant UnitedHealth Group has said it will acquire EMIS Group.
- The government called for evidence on discrimination within medical devices – based on patients’ social or demographic characteristics.
- NHS Digital published a new standard for creating online health content.
- NICE published Evidence standards framework (ESF) for digital health technologies.
- NHS Digital blogged about the lessons for IT projects from the COVID-19 home testing rollout.
- NHS Providers published the fifth part of its guide to boost board member’s confidence in digital: It set out principles for successful digital delivery and outlines practical take-aways for trust leaders, as well as a factsheet and highlighting key considerations that board members should be aware of when building and deploying digital services. The eight ‘how to’ principles are:
- Deliver things that patients and staff need
- Set clear, realistic goals
- Test, measure and learn how it is working
- Think long term, deliver short term
- Invest in a dedicated, cross-functional inhouse digital team
- Get the best out of technology suppliers
- Build trust not barriers
- Not sticking to the wrong plan.
IT policy: Integrated Care Systems (ICS)
- techUK published a report on What should ICS prioritise to make digital, data and technology work for them and their populations? (pdf report). The report was written in collaboration with techUK’s Health and Social Care Council, the supplier community. It includes case studies and five key recommendations for ICS. com reported on the techUK’s work.
- HSJ.co.uk opined on how ICSs could best benefit from digital technology.
- Better’s Chief Technology Officer commented on the digital challenges with ICSs achieving integrated care.
- Integrating Digital Health and Care 2022 webinars were made available as videos on-demand. These videos explored the digital innovation and integration taking place and the latest in the development of ICSs.
IT policy: health and care around the globe
- HealthcareITnews.com opined on What can Europe to do bridge the digital health divide.
- Weforum.org considered How can countries achieve digital maturity in healthcare. And compared digital maturity across multi countries.
- Apple set out its current and future plans for healthcare.
- Google faces a lawsuit regarding use of millions of UK citizen’s medical data.
- Amazon is set to acquire primary care tech provider, One Medical.
IT policy (future)
- Digitalhealth.net opined on What the end of Control Of Patient Information (COPI) emergency measure could mean for digital health innovation.
- Health Tech Trends hypothesised on what digital primary care will look like in two, five and ten years.
- Alcidion’s Chief Technology Officer argued that the future of health care systems may lie in open standards and open APIs.
- OpenAccessGov.org set out improvements that might be made to patient care through the use of technology.
- The Medical Futurist speculated about a possible increased role for lifestyle medicine.
Innovation
- PRSB launched the #CareAboutMe campaign to raise awareness of the About Me standard.
- Boots completed a test flight from Portsmouth to the Isle of Wight which involved prescription-only-medicines being delivered by drone.
- NHS is to pilot smart goggles for community nurses to free up their time.
- MHealthIntelligence.com explained What Are Digital Therapeutics and Their Use Cases?
- GPonline.com reported on NHS England piloting online patient registration for GP practices.
Genomics
- Pharmacy professionals were invited to use a new Genomics Centre for Pharmacy Postgraduate Education (CPPE) learning portal.
- A study suggested that Genome screening within Primary Care may be feasible.
- The NHS England Genomics team have produced draft and other materials:
- NHS England are consulting on their genomics strategy and what may be missing from it. The consultation is due to close 16th October 2022. Any CP ITG participants who are considering completing a consultation response may wish to consider the RPS position statement on ‘The Role of Pharmacy in Pharmacogenomics’.
IT policy (general)
- NHS England published its 2022/23 business plan which includes a “strategy for technology in health and care to digitise services, connect them to support greater integration and, with these foundations, enable service transformation”.
- Department of Health and Social Care published a plan for digital health and social care. Reactions to the plan included The King’s Fund; Sector; co.uk; and HealthcareITnews.
- Cala Health opined on the main drivers for patient adoption of digital health technologies.
- CP ITG published its Pharmacy IT quarterly round-up after the group’s last meeting.
- NHS Digital blogged about how their team working on the developer hub ensured that the hub would not exclude people with accessibility needs.
- NHS launched a review into the digital readiness of the nursing profession.
- Survey results suggested that half of NHS frontline staff respondents felt that the lack of tech investment is harming their wellbeing and their job performance.
- Health Tech Trends 2022 analysed survey results to identify what can we learn about digital transformation from the past year?
Interoperability and records
NHS Profile Manager
- Previously, community pharmacy contractors used two different NHS systems to ensure their pharmacy details were up to date in the Directory of Services (DoS) and on the NHS website: the NHS website profile editor and the DoS Profile Updater.
- A new tool, NHS Profile Manager launched to replace both the DoS Updater and the NHS website editor during late June 2022.
- A series of NHS Profile Manager video tutorials from NHS Digital can be used to support pharmacy teams with using the tool.
- Community Pharmacy England has been a member of the NHS Profile Manager steering group since June 2021 and continues to participate in related sub-groups to help with the project rollout and any deployment hurdles.
- Community Pharmacy England published a news item about use of NHS Profile Manager regarding the 19th September 2022 bank holiday.
- Multiples head office staff that use NHS Profile Manager should create a personal NHSmail account if they have not already done so. Advice is available within the ‘NHSmail personal accounts: creation and linking’ section of Community Pharmacy England’s NHSmail
- NHS Digital will be working with the pharmacy multiples regarding the NHS website and DoS Application programming interface (API).
- If the pharmacy team members want to discuss the potential enhancements on the wishlist, please contact it@cpe.org.uk.
Shared Care Records (ShCR): status
- Shared Care Records (ShCR), formerly ‘Local health and shared care records’, are patients’ electronic health records. ShCRs include information from multiple care settings, e.g. GP practice and secondary care. Most English patients live within an area with a records project ongoing. Shared care records are emerging across the country and the IT has been maturing so that over time more health and care professionals can access these. LPCs and/or local contractors can continue to take steps to gain pharmacy access and should use the guidance set out at the ‘Engagement’ section of the community pharmacy and ShCRs webpage.
- Community Pharmacy England published a new ShCR case study during July 2022: Somerset Shared Care Record case study (SIDeR). Digitalhealth.net reported that Somerset Integrated Digital ShCR is now being used 13,000 times a month (by a mixture of healthcare settings).
- Community Pharmacy England continues to work with the NHS Transformation Directorate and other relevant stakeholders on the actions set out within the Shared Care Record (ShCR/LHCR) NHS Transformation Directorate and pharmacy outputs and actions LPCs, ShCR project teams and other parties supporting ShCR pharmacy deployment are encouraged to contact it@cpe.org.uk with any technical ShCR information so that supplier and IT support helpdesks can authorize multiple ShCR domains simultaneously.
Records
- SCR AI changes continued beyond COVID-19 legislation which expired at the end of June 2022. Community Pharmacy England and the Community Pharmacy IT Group have campaigned for pharmacy teams’ access to SCR AI to be extended beyond the pandemic by sharing case study information. If you have any examples of how SCR with AI has enhanced patient care, in comparison to the normal SCR access, please contact it@cpe.org.uk, as such examples could be used to support the case for permanent access to SCR with AI and other health records for pharmacy.
- Community Pharmacy England conducted some interviews with pharmacists that frequently used ShCR systems. Some of the comments about ShCR and GP Connect Access Record included the below:
- If there is integration with both, this provides continuity if one system experiences an outage.
- ShCRs and GP Connect each have some of their own benefits and challenges.
- ShCR records can include structured information from across multi sectors e.g. helping with the delivery of Discharge Medicines Service (DMS) when discharge information can reach the pharmacy before the GP Practice.
- GP Connect records are useful for a lot of dispensing work, but record data from other settings does not always impact the GP record swiftly and in a structured way.
Standards and interoperability
- NHS Digital’s Programme Head for GP Data outlined the benefits and challenges of health data sharing.
- At a previous CP ITG meeting, the group agreed to support the capability for anonymised data to be accessible, so that pharmacy teams’ interventions can start to be auditable, and the value of community pharmacy can be better demonstrated. If PMR systems were to be adapted to allow such data sharing, it would require the development of a roadmap and a standard approach to data provision, which may benefit from use of SNOMED CT clinical terms. If you would like to help with this work, please contact it@cpe.org.uk.
Recommended minimum transfer dataset for pharmacies switching from one patient medication record (PMR) system to another
Community Pharmacy England previously supported developing a recommended minimum dataset for cases where a pharmacy contractor has switched from one PMR system to another. For the sake of continuity of patient care, it is critical for some patient information to be transferred from the old to the new system. A dataset is being developed incorporating the previous comments. An associated specification document is also being developed. A working group of supplier representatives chaired by Community Pharmacy England has conducted monthly meetings to discuss the detail of the proposed documents. This work is identifying areas where PMRs may wish to consider future proofing by exploring opportunities to align the way data is stored within the local PMR to various national standards. Community Pharmacy England is aligning this further with individual NHS data dictionary standards to support the next steps. The working group is to meet again once the dataset is further developed.
NHSmail
- User research into NHSmail and authentication: Multi-Factor Authentication (MFA) provides additional security for digital access. Good data security practices require use of individual logins for different persons and consideration of MFA where needed. Microsoft enables MFA for Outlook as an option. NHS Digital are considering the impact of MFA on NHSmail users, e.g. a recognised phone confirms the access at a relevant interval (not necessarily for every login). The group was asked to share views about MFA and any associated pharmacy requirement if this was to be introduced. Pharmacy team members can send comments about the proposed introduction of multi-factor authentication to enable use of NHSmail to it@cpe.org.uk.
- The Virtual Visits tool provides pharmacy contractors with an appointments system so that they can notify patients and better manage appointments. Pharmacy teams can also use the Virtual Visits tool to conduct face to face or virtual patient consultations (audio or video).
- The Virtual Visits tool works in conjunction with NHSmail Microsoft Teams and the Microsoft Booking platform. To participate in the pilot, you must have an active personal NHSmail account, access to a shared NHSmail inbox, MS Teams installed on a computer or tablet and a computer or device with a webcam. Contractors that have not done so should register interest with taking part in the Virtual Visits pilot via this webform.
- Since the recent launch of the NHS Profile Manager tool, which uses NHSmail accounts to allow pharmacy team members to login to it, both Community Pharmacy England and the NHSmail team have received an increasing number of questions from pharmacy contractors regarding NHSmail. A selection of NHSmail queries that have been submitted by contractors are available within a new Community Pharmacy England NHSmail FAQs briefing factsheet.
IG, identity and security
Data Security and Protection Toolkit (DSPTK)
Community Pharmacy England updated its Data security and information governance hub and published new guidance for the 2021/22 Toolkit submission. Additionally, Community Pharmacy England and NHS Digital jointly presented a webinar on the topic, with around 500 people registered to attend the webinar on the night. The webinar was subsequently made available on demand. Community Pharmacy England and NHS Digital are working on the arrangements for the community pharmacy toolkit publication ahead of the next June 2023 deadline. If you would like to feed into the development of the 2022/23 toolkit, please email it@cpe.org.uk.
Other data security updates
- NHS Digital blogged about how networking, and the NHS Cyber Associates Network (CAN), plays a part in mitigating cyber threats.
- The UK government called for views from the tech industry on enhanced security and privacy requirements for firms running app stores and developers making apps. The UK government’s review into the app store ecosystem from December 2020 to March 2022 found that malicious and poorly developed apps continue to be accessible to users, therefore it is evident that some developers are not following best practice when creating apps.
- The National Cyber Security Centre (NCSC) published a report on app store risks.
- A cybersecurity expert considered the ransomware attacks threatening the NHS.
- HSJ.co.uk provided tips about building resilience against major cyber-attacks.
Reducing burden
- NHS Digital ran wireless tech trials to improve health and care service processes.
Usability
- NHS Digital blogged about a new approach to supporting product development involving measuring the development team’s maturity.
- NHS Digital blogged about Why creating an online service is more than just digitising a form.
Development of pharmacy systems
NHS Digital update on CPCS minor illness post event structured message
NHS Digital technical specification is being worked on: https://digital.nhs.uk/developer/api-catalogue/digital-medicine-fhir.
Professional Record Standards Body (PRSB) progress
Community pharmacies now offer an expanded range of services to support patients and members of the public. The Professional Record Standards Body’s (PRSB’s) Community Pharmacy Data Standard defines the subset of information that should be sent to the GP record for specific services. NHS Digital has now updated its information about notifications from pharmacy to GP systems using the Community Pharmacy Data Standard.
Core Information Standard and records standards: PRSB is consulting on updates to Core Information Standard.
111 referral as part of Booking and Referral Standard (BaRS) for 111 to community pharmacy:
- PRSB has created a standard to support clear and concise information flows between the 111 referrer and the receiving services and professionals or clinicians to support safe and effective care. The standard defines the information that should be shared from 111 or 999 services when a person is referred onto another service.
GP Online Consultation referral to community pharmacy: GP online consultation referrals to community pharmacy will launch from October 2022 within a London pilot guided by existing PRSB standards.
Work to revise and future-proof the Community Pharmacy Data Standard: PRSB anticipates further work for the Community Pharmacy Data Standard.
PRSB Standards Partnership Scheme: The PRSB Standards Partnership Scheme connects the PRSB with clinical system suppliers to accelerate development, adoption and implementation of PRSB standards. Many suppliers who have joined the scheme have undertaken conformance assessment to receive the PRSB Quality Mark, demonstrating that their systems are standards compliant to their users and commissioners. This process has its advantages for system suppliers and for PRSB standards, for example, it has helped PRSB to consider adaptation of standards to smoothen the implementation journey for suppliers. The scheme may work well for community pharmacy system suppliers, e.g. implementation of Community Pharmacy Data Standard.
PRSB professional network: PRSB have launched a new Professional Network for any individual working in the health or care sector with an interest in standards and the digital agenda. Pharmacy professionals may consider registering to participate within the PRSB professional network.
PRSB running a campaign to support use of the ‘About Me standard’: PRSB’s ‘#CareAboutMe’ campaign aims to raise widespread awareness of the About Me standard and the improvements this can make to the quality of care administered in health and care, as well as the positive impact this could have on people’s quality of life and health. About Me information is the most important details that a person wants to share with professionals in health and social care.
Diabetes information care record standard: The new standard on Diabetes information care is split into two parts: the first covering the information that people treating diabetes and people with diabetes would want to be able to see, enabling sharing of this information between all the different setting of those involved in the care. The second concerns self-management standards from people’s own personal devices.
Projects in development or being updated: Maternity, wound care, workforce, anaesthetic charts, end of life, diabetes standard and social prescribing.
CPCF IT Toolkits and Future Enterprise Architecture for pharmacy IT systems
NHS England has commissioned work to create technical toolkits to support the development of IT for CPCF clinical services. Four IT toolkits (Discharge Medicines Service, New Medicine Service, Blood Pressure Check Service, Smoking Cessation Service) are undergoing final internal sign off and publication approval. These will be hosted on the NHSBSA website. NHS Digital has recommended Future Enterprise Architecture for community pharmacy IT systems. Suppliers may review the information about Future Enterprise Architecture and associated prerequisites.
Pharmacy Contraception Service technical toolkit
The Pharmacy Contraception Service will be commissioned as an Advanced service from 11th January 2023 following the pilot. The drafted Pharmacy Contraception Service technical toolkit will be further published shortly.
GP Connect and other record systems
GP Connect enables GPs and other authorised health care organisations to link in with GP system information, enabling those authorised to use functionality including “Access Record”. The GP Connect Access Record programme allows authorised clinicians access to GP patient records in a HTML read-only format or an editable format. The GP Connect Access Record programme allows authorised clinicians access to GP patient records in a HTML read-only or an editable format.
Electronic health records event
The CP ITG, together with NHS England’s Transformation Directorate, are hosting a Connecting with & benefitting from patient records webinar on Thurs 8th December 2022, 9.30am-11am. This event for LPCs and those with an interest in the records agenda will be focused on the future of records and how contractors’ access to Shared Care Records (ShCRs), GP Connect Records and other records can be improved. All CP ITG attendees and LPC Chief Officers are encouraged to attend. LPC members and contractors with an interest in improving contractor access to records are encouraged to also register to attend this event.
NHS England and Community Pharmacy England have been keen for suppliers to be given information about the service, including the IT implications and dataset requirements. NHSBSA and NHS England have further developed the Hypertension case-finding (Blood Pressure Check) and Discharge Medicines Service (DMS) Manage Your Service (NHSBSA MYS) APIs. The NHSBSA has issued this to suppliers. Suppliers have been invited to share any feedback with NHSBSA by email (nhsbsa.mys-platform@nhs.net). NHSBSA continues to encourage suppliers to share feedback if they have not already done so. Only one supplier has shared substantive feedback with the NHSBSA so far. The API documents for these services will help the future development of other API documents.
Booking and Referral Standards (BaRS) and appointments IT
NHS Digital’s BaRS programme aims to enable booking and referral information to be sent between NHS service providers in a format useful to clinicians. The intention is that BaRS will eventually be available in all care settings. Pharmacy use cases for the standard are currently being considered – including the potential for referrals from NHS 111 to community pharmacy. NHS England’s Transformation Directorate IT standards roadmap highlights BaRS as a priority.
The BaRS formal standard was published in June 2022, starting with a standard deployed for use between NHS 111 and emergency departments, 999 and Clinical Assessment Services, and at other key interfaces in the urgent and emergency care system (target date March 2025). The Pharmacy Integration team, along with others such as the Community Pharmacy IT Group, are supporting the development of pharmacy use cases.
The NHS Digital BaRS user research team are conducting interviews with health and care staff to inform the programme of work and support future business cases for expansion of the standard. Community Pharmacy England and NHS Digital are encouraging community pharmacy teams to share their views about bookings and referrals. The BaRS team would like to hear the view of pharmacists, pharmacy technicians, dispensers and pharmacy counter assistants. To date, the feedback submitted has only been from pharmacists. The BaRS team are conducting interviews (usually lasting 30-45 minutes) to hear more about the current experiences and the future preferences concerning sending and receiving referral messages.
CP ITG feedback has indicated that the BaRS programme should be expanded to incorporate NHS appointments standards.
An event will occur: CP ITG call BaRS user research call: 27th October 11am-11.45am. Pharmacy team members may contact it@cpe.org.uk to receive an invitation.
Cancer referrals pilot
The NHS Long Term Plan committed to increasing the proportion of cancers caught early, when they are easier to treat, from half to three in four. NHS England previously created a plan for pilots. The NHS e-Referral Service (e-RS) tool is expected to be evaluated during the piloting.
Vaccinations, the NHS National Booking Service and appointments standards
Following patients booking COVID-19 vaccination appointments via the NHS National Booking Service (NBS), NHS England are running a ‘proof of concept’ to explore expanding NBS into community pharmacy trial sites to enable patients to book seasonal flu vaccination appointments. The group will set-up a CP ITG call about Vaccinations, the NHS National Booking Service and appointments standards: 12th October 10.30am-11.15am. Pharmacy team members who would like an invitation may contact it@cpe.org.uk.
EPS and RTEC
Electronic Prescription Service (EPS)
- NHS Digital EPS and eRD utilisation rate statistics (for the May 2022 dispensing month) are set out on the right.
- NHS Digital would like to talk to pharmacy team members about their experience using EPS. User feedback is essential to inform future improvements and the next generation of the system. Please could pharmacy EPS users within the group take part and provide views, by signing up at https://feedback.digital.nhs.uk/jfe/form/SV_eu4jQRNbJooQxoO. This may involve a short telephone interview.
- The content on the eRD page of the Community Pharmacy England website has recently been fully refreshed. Alongside the updated content on the webpage, several new materials have been published, covering:
- LPCs will soon receive a regular breakdown of eRD performance within their area from Community Pharmacy England.
- NHS Digital is conducting a review of EPS nomination reporting. The review will involve a data cleanse, removing nominations which are of deceased, superseded, invalid, and test patients from the reported figures. The date of this change will be Monday 3rd October 2022. The change will affect the count of nominations only – the format of the data will remain unchanged.
- The EPS team continue to work on EPS FHIR API. The EPS Tracker REST API remains in Beta. In regards to other EPS APIs: EPS HL7 V3 API remains stable, and the EPS Directory of Services API is under review and NHS Digital are considering deprecating it.
Real Time Exemption Checking (RTEC)
- The NHSBSA continues to lead the RTEC project. The NHSBSA, DWP and the RTEC steering group plan has supported the expansion of the DWP RTEC functionality to additional pharmacy contractors. Community Pharmacy England communicated during July 2022 that RTEC DWP roll-out had reached over 80% of pharmacies. Contractors using RTEC should now be able to use the RTEC DWP feature. Community Pharmacy England and other RTEC steering group members are exploring what should be added to the RTEC roadmap. Examples requested before included:
- if patient updates address at GP, NHSBSA get this, to reduce RTEC unknowns confirmed instead of ‘RTEC yes’
- patients have a ‘checker’ which uses same info as presented in RTEC, to reduce scenarios where patient believes must pay charge, but PMR says ‘RTEC yes’
Note: Both these examples would require significant technical change to be addressed. Dan Ah-Thion will ask the group whether there are additional items which should be considered for the RTEC roadmap. Pharmacy team members may send further items for consideration for the RTEC development roadmap to it@cpe.org.uk.
Smartcard admin portal
Currently pharmacy contractors use the Care Identity Service (CIS) portal to administer their NHS Smartcards. Example functionality includes the ability to register to be able to ‘self-unlock’ and the ability to request new Smartcards. The Care Identity Management (CIM) portal is being developed so that more Smartcard users can use the portal to administer their Smartcards. The current plan is to close the CIS portal, and to transition Smartcard users to the CIM portal. Pharmacy contractors and team members are encouraged to participate in user research by emailing iamplatforms@nhs.net using the subject title “CIM research”.
NHS Digital and Community Pharmacy England are seeking additional feedback from pharmacy teams about the existing portal:
- How do and your teams you usually go about unlocking Smartcards?
- What do you think could be improved?
Smartcard identity checking process to be digitised: Apply for Care ID
Pharmacy team members must authenticate their identities to be linked to their Smartcards. Prior to the pandemic, pharmacy team members had to attend face-to-face meetings with local Registration Authority (RA) staff. The NHS implemented emergency policies throughout the pandemic so that staff could authenticate themselves remotely, e.g., via video calls. These emergency policies will end shortly.
NHS Digital hopes that a successful pilot will lead to the rollout of ‘Apply for Care ID’. This programme will enable health care staff use an NHS authenticator app as an alternative to a face-to-face visit to the RA. The service has been in pilot since April and the project team has incorporated feedback from Community Pharmacy England in their plans. Further pilot work will involve participating organisations (including pharmacy contractors) inviting individuals to go through the steps. Extra pharmacy team and head office views are needed to support the discovery and business cases for a process which could involve pharmacy teams being given an offer to authenticate themselves via a phone app. The pilot learning should consider technical aspects (device standards, browser standards and public cloud access), procedural aspects (what documentation is required), and the people aspects. The previous quarterly bulletin set out additional developments about Apply for Care ID.
Pharmacy contractors and team members are encouraged to participate in the user research by emailing iamplatforms@nhs.net using the subject title “Apply for Care ID research”.
Smartcard self-unlock process and guidance
NHS Digital have been updating their Smartcard guidance ahead of sharing this refreshed guidance with the CP ITG: https://digital.nhs.uk/services/registration-authorities-and-smartcards/register-for-self-service-smartcard-unlock. Pharmacy teams are encouraged to familiarise themselves with the guidance.
Drug Tariff IT and dm+d code changes
Community Pharmacy England and the Department of Health and Social Care will set up some workshops.
- CP ITG Drug Tariff IT call October 11th 1pm-2pm. Pharmacy team members, or others who would like to attend, may contact it@cpe.org.uk.
- CP ITG dm+d medicine code changes call October 12th 9.30am-10.15am. Invitations will be sent to CP ITG. Supplier representatives or others who would like to attend, but do not yet have an invitation, may contact it@cpe.org.uk.
Apps, wearables and technologies (incl videocon)
NHS App
- NHS Digital blogged about how suppliers could start to more easily integrate with the NHS App.
- The NHS App team are continuing to work on existing and future features including:
- Booking or managing a vaccination – Currently patients can book or manage their vaccination appointments using the National Booking Service. As part of this service, they are required to answer questions about their health circumstances and are then offered a vaccination appointment based on the results.
- Personal Health Records integration with the NHS App.
- Notifications and messages direct to the NHS App: a pilot with 7 GP practices was concluded successfully with positive feedback from members of the public, GPs and communication service providers. Messages could include reminders for appointments or online consultations.
- Access to GP health records. From late 2022, patients with online accounts such as through the NHS App will be able to read new entries in their health record. This applies to patients whose practices use the TPP and EMIS systems.
NHS account
- The NHS website has adjusted its use of terminology used regarding accessing certain NHS services online. The NHS website now call this ‘logging into the NHS account’, whether by NHS App or the NHS website.
- Community Pharmacy England updated its information about NHS account.
- The NHS account team provided updates about the changes made to NHS account functionality. This includes the latest updates, bug fixes and new features. See: NHS account release notes.
NHS Profile Manager
- Previously, community pharmacy contractors used two different NHS systems to ensure their
pharmacy details were up to date in the Directory of Services (DoS) and on the NHS website: the
NHS website profile editor and the DoS profile updater. - A new tool, NHS Profile Manager was launched to replace both the DoS Updater and the NHS
website editor. - Community Pharmacy England has participated within the NHS Profile Manager steering group since June 2022 and related
sub-groups to support the project, preparatory work and the current launch. - A CP ITG sub group attended two demo meetings, both of which have were recorded and posted
online: CP ITG Profile Manager Demo and meeting video 1 (December 2021); and Demo and
meeting video 2 (February 2022). The group also discussed the future enhancements with NHS
Profile Manager team.
Next steps:
- In February, Community Pharmacy England published communications about progress with the launch and further
communications are expected before or just after the group’s June 2022 meeting. The group and
contractors are encouraged to support the cascade of messages. - Multiples head office staff that use NHS Profile Manager should create a personal NHSmail
account if they have not already done so. Advice is available within the ‘NHSmail personal
accounts: creation and linking’ section of Community Pharmacy England’s NHSmail webpage. - NHS Digital will also be working with pharmacy multiples regarding the NHS website and DoS
Application programming interface (API). - If the group or contractors wish to discuss potential enhancements on the wishlist, please contact
it@psnc,org.uk.
Shared Care Records (ShCR) update
- LPCs and/or local contractors that want to gain pharmacy access to such records should:
o identify their ShCR project team from the List of records systems (this list was recently
updated);
o read case studies such as Dorset Care Record ShCR pharmacy access case study and the
East London Patient Record (eLPR) pharmacy case study;
o contact the ShCR project team and local partners to find out how to get involved;
o Make use of the ‘Planning pharmacy access briefing’ and ShCRs webpage; and
o review the previous Community Pharmacy England/RPS ShCRs/SCR letter to NHS orgs about records access. - Community Pharmacy England continues to work with the NHS Transformation Directorate and other relevant
stakeholders on the actions set out within the Shared Care Record (ShCR/LHCR) NHS
Transformation Directorate and pharmacy outputs and actions documents. LPCs, ShCR project
teams and other parties supporting ShCR pharmacy deployment are encouraged to contact
it@cpe.org.uk with any technical ShCR information so that supplier and IT support helpdesks
can authorize multiple ShCR domains simultaneously. - CP ITG representatives including Community Pharmacy England, CCA, NPA and supplier reps attended several events
hosted by the Professional Record Standards Body (PRSB) regarding Accelerating shared care
records (March 2022), Driving standards (June 2022), two Core info standard workshops (June
2022) and a June meeting about draft pharmacy ShCR guidance from the NHS. Community Pharmacy England and CP ITG
attendance was to support the ShCR agenda and progression. - A CP ITG pharmacy records event will be held in mid-October 2022 for the group, Local
Pharmaceutical Committee Chief Officers, ShCR/GP Connect teams and others. Work will be
undertaken ahead of this.
Records
- SCR AI changes to continue beyond COVID-19 legislation. Community Pharmacy England and the Community Pharmacy IT
Group have successfully campaigned for pharmacy teams’ access to SCR AI to be extended
beyond the pandemic by sharing case study information. Community Pharmacy England and the Royal Pharmaceutical
Society both wrote to the relevant authorities within the NHS to share the significant evidence
highlighting how SCR AI access for pharmacy teams improves patient safety. However, NHSE&I is
still considering a permanent policy change. If you have any examples of how SCR with AI has
enhanced patient care, in comparison to the normal SCR access, please contact it@cpe.org.uk,
as such examples could be used to support the case for permanent access to SCR with AI and
other health records for pharmacy. - The UK Health Secretary called for 90% of NHS trusts to use electronic patient records (EPR) by
2023. - The supplier, accuRx launched a national patient-centred record viewing system.
- A poll indicated growing acceptance of technology in NHS: Nearly two thirds (61%) of patients
reported that they are comfortable with GP appointments over the phone or via video calls, which
was one of the changes introduced to maintain social distancing and stop the spread of
Coronavirus during the pandemic. Three in five (60%) patients are satisfied with their local
engagement with the NHS (for example, a consultation with their GP) since the outset of the
pandemic, and 69% of patients rated the performance of the NHS since the pandemic as either
good or excellent. - Twenty-five of the least digitally mature NHS trusts are to be prioritised for future investment in
electronic patient records (EPRs).
Standards and interoperability
- NHS Digital introduced interactive maps to their NHS Service Finder online search tool. Community Pharmacy England fed
comments into the project team regarding the feature ahead of launch. - NHS Transformation Directorate published a draft standards and interoperability strategy with
the aim of driving interoperability across the NHS and social care. A consultation response was submitted from CP ITG to NHS Transformation Directorate’s about interoperability drawing from
the group’s meeting session about interoperability priorities during November 2021. - At a previous meeting, the group agreed to support the capability for anonymised data to be
accessible, so that pharmacy teams’ interventions can start to be auditable, and the value of
community pharmacy can be better demonstrated. If PMR systems were to be adapted to allow
such data sharing, it would require the development of a roadmap and a standard approach to
data provision, which may benefit from use of SNOMED CT clinical terms. A PSNC-drafted dataset
was prepared and a dataset for the Community Pharmacist Consultation Service (CPCS) could be
added. If you would like to help with this work, please contact it@cpe.org.uk. - NHS Digital outlined how ISO 13407 the user centric design standard could help suppliers.
- NHS Digital blogged about how they were making it easier for their APIs to be used.
- NHS Digital blogged about how their effort to put user needs at the centre of our API
documentation. The proposed work with suppliers should include: user research (including
sessions to watch how suppliers could find and use standards); web page feedback; a well-managed support mailbox managed by the project team; Interactive backlog; and regular surveys.
Booking, referrals and appointments (with IT)
- Community Pharmacy England is encouraging pharmacy teams to support the development of the new NHS Booking and
Referral Standard and take part in user research. NHS Digital is inviting community pharmacy
teams to share views relating to the new Booking and Referral Standard (BaRS). This will ensure
that the tool supports the needs of pharmacy team members and their patients. BaRS is an
interoperability standard for healthcare IT systems which should enable booking and referral
information to be sent to or from care providers quickly, safely and in a format useful to clinicians.
If you would like to take part or have any questions, please contact it@cpe.org.uk and/or
bookingandreferralstandard@nhs.net. - Community Pharmacy England has updated its webpage: Booking, referrals and appointments (with IT within pharmacy).
Supporting NHSmail
- Community Pharmacy England has published a new factsheet about using shared NHSmail inbox within the Outlook mobile
app for community pharmacy teams. - The Virtual Visits tool provides pharmacy contractors with an appointments system so that they
can notify patients and better manage appointments. Pharmacy teams can also use the Virtual
Visits tool to conduct face to face or virtual patient consultations (audio or video). - The Virtual Visits tool works in conjunction with NHSmail Microsoft Teams and the Microsoft
Booking platform. To participate in the pilot, you must have an active personal NHSmail account,
access to a shared NHSmail inbox, MS Teams installed on a computer or tablet and a computer
or device with a webcam. - Virtual Visits can be piloted by many more contractors (potentially circa 100) across summer
2022. Contractors that have not done so should register interest with taking part in the Virtual Visits pilot via this webform. - Multi-Factor Authentication (MFA) provides additional security for digital access and the
NHSmail team has been asked to explore the implications, benefits and impacts with MFA
introduction for health and care NHSmail users. The group is asked to share views about
NHSmail MFA and any associated pharmacy requirement to it@cpe.org.uk.
Data Security and Protection Toolkit (DSPTK)
- Community Pharmacy England issued communications and guidance relating to the completion of this year’s Toolkit.
- Community Pharmacy England again worked closely with NHS Digital and contractor testers to keep the workload manageable but the data security protections appropriate. The key differences included the addition of new mandatory questions and improvements to the wording of all the questions.
- Community Pharmacy England updated its Data security and information governance hub during April 2022 to support Toolkit completion and published new guidance for the 2021/22 Toolkit submission including:
o Toolkit completion: Five steps to complete the Toolkit (overview)
o Toolkit completion: Question-by-question guidance (mandatory questions) - Community Pharmacy England’s data security templates have all been updated: cpe.org.uk/dstemplates.
- A training option was revised: Pharmacy data security (for induction or refreshment).
- Community Pharmacy England has also hosted meetings with the PMR suppliers and NHS Digital, to help the PMR suppliers with their preparation of PMR-specific guidance for contractors.
- Community Pharmacy England and NHS Digital jointly presented a webinar. Around 500 people registered to attend the
webinar on the night. The webinar was made available on demand.
Next steps:
- If you would like to feed into the development of the proposed 2022/2023 question set, please
email it@cpe.org.uk.
Internet Explorer support coming to an end, Care Identity Service and NHS Credential Management
(particularly relevant for pharmacy IT support)
- Microsoft announced a long time ago support for Internet Explorer (IE) 11 is to be withdrawn from June 2022.
- Community Pharmacy England, and NHS Digital teams met to discuss the impact on the community pharmacy sector.
- NHS Credential Management (CM), is a new component from NHS Digital that supports the move
away from IE (whether the browser itself or related IE plugins within other internet browsers).
CM is standalone installation, which facilitates communication between the Identity Agent and
modern browsers, removing the dependency on Java Applets and IE11. - NHS Credential Management also replaces current card management system operations within
the NHS Care Identity Service (CIS) user registration service. - NHS Spine user tools such as SCRa and EPS Prescription Tracker are now CM compatible. By
removing the requirement for applets and unsupported browsers, CM facilitates improved security and performance. CM is a required installation as part of the transition to CIS2 Authentication. - CIS1 is anticipated to shift into a sunset phase, with a deprecation date of September 2023. It is
anticipated CIS2 benefits could include potentially enabling the move away from reliance only on
physical Smartcards. Pharmacy system suppliers are currently engaged with the NHS CIS2 team,
but if a system suppler requires further information they should contact nhscareidentityauthentication@nhs.net and may also flag issues at their catch-ups with NHS
Digital / EPS team / NHSBSA. - IT support may consider installation of NHS Credential Management onto community pharmacy
machines where necessary. It is not recommended that contractors install components onto their
machines without liaising with their IT support.
Other data security updates
- Community Pharmacy England reported on the National Cyber Security Centre (NCSC) urging organisations to bolster their
cyber security resilience in response to the malicious cyber incidents in and around Ukraine. - The National Data Guardian (NDG) published ‘The right to privacy; digital data’.
- NDG published the minutes from their panel meeting. These minutes indicate that there will be
guidance for exit from the Control of patient information (COPI) notice – scheduled for the end of
June 2022. - Microsoft announced Windows 11 plans. Many Windows 10 users are currently eligible for a free
upgrade to Windows 11, provided that the computer meets the strict minimum system
requirements (e.g. 64-bit processor and 4GB RAM). Pharmacy contractors are advised not to
update their machines without the agreement of or supervision from their IT support. Read more:
CP ITG: Windows briefing. - The IT supplier, Specops explored the human side and the technology side of why passwords can
be seen as the weakest link in an organisation’s network.
Smartcard identity checking process to be digitized
- NHS Digital are exploring improved processes regarding face-to-face authentication checks for
pharmacy team members to update their Smartcards – via a new NHS Digital product: Apply for
Care ID”. Extra pharmacy team and head office views are needed to support the discovery and
business cases for a process which could involve pharmacy teams being given an offer to
authenticate themselves via a phone app. - This new programme involves health care staff being given the opportunity to use an NHS
authenticator app as an alternative instead of a face-to-face visit to the local Registration
Authority. The group and contractors are encouraged to participate with user research (including
feeding back regarding what authentication is necessary within community pharmacy e.g.
whether or not NHSmail and Disclosure and Barring Service checking is required or not) by
volunteering to take part in interviews by contacting iamplatforms@nhs.net ccing it@cpe.org.uk. - NHS Digital previously added the multi-site ‘FFFFF’ Smartcard code and SCR rights onto
Smartcards with the pharmacist or pharmacy technician role, because of the COVID-19 pandemic.
This initiative was supported by Community Pharmacy England and NHSE&I. NHS Digital previously confirmed to Community Pharmacy England that assignment codes are further extended until 31st March 2022. This has been further extended.
Community Pharmacy England is in discussions with NHS Digital about the benefits of this innovation irrespective of the
pandemic and the benefit with disentangling this from the Control of patient information (COPI)
notice.
Paperless
- The group previously identified going paperless as a priority – within its Digital Priority List and
Views on the next generation of EPS shortlists. However, pharmacy teams continue to report
considerable use of paper and printing for reasons such as enabling prescription information to
move around the dispensary given limited space for PMR terminals. Following work with the
group and the paperless sub-group the ‘Going paperless’ webpage is now available. - Since the April 2022 dispensing month, the NHSBSA Manage Your Service (MYS) system has been
the route for monthly FP34C submissions instead of the legacy paper submission method. This
has also enabled speedier payments to be made to those contractors who submit promptly.
Data
- Community Pharmacy England published a new webpage: Keeping your pharmacy profile information up-to-date. When
information about pharmacies changes, there are multiple profiles to be updated (aside from NHS
website and DoS). Regular updates and corrections will help ensure that others will be able to
contact or visit the pharmacy as needed. - Community Pharmacy England updated its webpage about the NHS Parent Organisation Code (POC). POC is the pharmacy’s unique identifying code for the parent organisation. Every pharmacy contractor has a POC even if there is one pharmacy within the organisation. There is a process to make corrections if required. The POC was utilised to help enable the running of the summer 2022 Pharmacy Representation Review Steering Group (RSG) meeting.
- The NHS Transformation Directorate, NHS Digital, Community Pharmacy England and others are supporting an initiative to rationalise central lists of pharmacy data used within NHS systems and datasets. This will help
align data, reduce pharmacy workload, and improve accuracy and data quality. The workstream
is also helping to identify future NHS Profile Manager enhancements, some of which are being
added to the roadmap.
Discharge Medicines Service (DMS) Manage Your Service (MYS) API
- DMS was introduced as an Essential service last year. NHSE&I and Community Pharmacy England have been keen for
suppliers to be given information on the service, IT implications and dataset requirements. There
is an objective to progress the integration work further. Some of this progress is dependent on
NHSBSA and supplier preparations. NHSBSA shared an updated specification to suppliers in June
2022. NHSBSA will further engage with suppliers for comments during summer 2022. Supplier
alignment to the specification could ease burden relating to pharmacy double data entry.
CPCF IT: Toolkits
- At previous meetings, the group agreed that they supported the CPCF specifications and felt that
the group should provide comments on these specifications. NHSE&I has commissioned work to
create technical toolkits. These toolkits have recently been published in draft format for: Blood Pressure Check technical toolkit, Smoking Cessation technical toolkit, Contraception
Management technical toolkit, Discharge Medicines Service technical toolkit and New Medicine Service technical toolkit. CP ITG representatives have been notified before the group’s June 2022
meeting. - Suppliers, the group and contractors should feed back to NHSE&I and also can feed back to
it@cpe.org.uk to comment onto the CP ITG collated comment. NHSE&I are conducting workshop
calls and inviting suppliers along to these and to feed into changes to the drafts. Suppliers can express interest with aligning to these toolkits by emailing NHSE&I commercial hub (or contacting
it@cpe.org.uk if email address info required).
GP Connect
- GP Connect enables GPs and other authorised health care organisations to link in with GP system
information. GP Connect enables those authorised to:
o Access records: GP Connect lets authorised clinicians access GP patient records in a HTML
read-only format or within an editable format;
o Send Documents: the tool enables GPs and other healthcare professionals to update a
patient record via ITK3, and MESH message; and
o Appointment Management: GP connect enables the sharing and management of
appointments. - The ‘GPC records’ programme enables health care staff to access GP records information if
suppliers have integrated into GPC. The integration processes have eased during the last year.
Recommended minimum transfer dataset for pharmacies switching from one patient medication record (PMR) system to another
- The group previously supported developing a recommended minimum dataset for cases where
a pharmacy contractor has switched from one PMR system to another. A previous draft iteration
version was supported by the group. For the sake of continuity of patient care, it is critical for
some patient information to be transferred from the old to the new system. - A drafted dataset has been prepared incorporating the comments from previous group meetings
and suppliers. An associated specification document has also been prepared. The dataset does
not include all the records within pharmacy systems but is intended to be a starting point as to
strengthen data quality. Suppliers recently requested changes, including:
o arranging the data into tables instead of within a data block (via JavaScript Object
Notation (JSON) format); and
o categorising the data by Medicines, Patient, Prescriber and Prescribing Organisation. - A working group of supplier representatives and Community Pharmacy England has been meeting every two weeks to
progress the proposed documents. This work is also identifying areas where PMRs may wish to
consider future proofing by exploring opportunities to align the way data is stored within the
local PMR to various national standards.
Supporting systems
- The group previously published its “Use and development of pharmacy systems – Suggested
features list v1.0”. Feedback has led to this being updated. The updated list will be published
during late 2022. See: “CP ITG- Use and development of pharmacy systems – Suggested features – comments.docx. - System suppliers previously fed back that several projects were ongoing or forthcoming within
the NHS (see: Gantt Chart (slide) and spreadsheet version). A group of system suppliers prepared
a letter addressed to NHSE&I, and other pharmacy IT policy makers to explain the benefit of
advanced IT project planning with regards to enhancing pharmacy teams and patients’
experiences. The letter was distributed after the CP ITG group’s previous meeting and a copy was
published online. NHS policy makers have since provided a reply to the letter (see below).
Supplier letter
Dear System Supplier leads,
Further to our letter in April we hope that this subsequent letter provides some of the additional detail as promised, and more importantly that this letter evidences our intention to keep this conversation with you open in order that we can support the ambitions of the sector and ensure we can collectively deliver the digital capabilities required to support the vision set out in the Community Pharmacy Contractual Framework (CPCF) for community pharmacy to play an increased role in the delivery of primary care, delivering more services, in safe and efficient ways, for patients .
Working collectively, the NHS Business Services Authority (BSA), NHS Digital (NHSD), the Department of Health and Social Care (DHSC) Pharmacy Team and both NHS England and NHS Improvement (NHSEI) Transformation Directorate and Pharmacy Team, have defined what we believe to be the ‘Top 5’ digital priorities for the community pharmacy sector over the next 22 months. This will take us to April 2024, the end of the current transformative five-year CPCF.
For system suppliers that are supporting the Electronic Prescription Service (EPS):
- Development against the Electronic Prescription Service API (next generation). EPS is currently the de-facto mechanism by which primary care prescriptions are sent to dispensers so patients can receive their medication. A range of improvements to the service have been identified and a programme has started to design and develop core changes that will modernise the service, allowing innovation for new capabilities and reducing system development time. A new fully FHIR based service is being developed which will improve the user experience for prescribers, dispensers and patients alike. The work will support a further reduction in paper and provide a modern, flexible EPS. We are working with dispensing system suppliers to support their development and will develop central capability to support the live service during the transition to the new infrastructure. We anticipate readiness engagement with system suppliers to commence in Q4 of 2023. For further information please contact interopmeds@nhs.net.
For system suppliers that are offering or want to offer the system functionality to support the delivery of community pharmacy clinical services as per the current CPCF:
- Compliance with the Professional Records Standards Body (PRSB) Community Pharmacy Data Standard to enable information about services provided by community pharmacies to be recorded and transferred in a safe and efficient manner to their GP practice. The standard was first published by PRSB in 2018 and uplifted in 2021 to meet the full requirements of the CPCF. Further information regarding supplier conformance is available from the PRSB. NHSD are preparing the technical specification to develop interoperability between community pharmacy and GP systems and expect it to be available to suppliers by September 2022.
- Access to patient care recordsWe are aware that a number of system suppliers have already enabled pharmacy contractor access to patient care records through integration with the Patient Demographic Service (PDS) and 1-click access to the Summary Care Record (SCR).For the duration of the coronavirus (COVID-19) pandemic, contractors had access to SCR additional information to help support clinical decision making. This access is to continue while permanent policy changes, taking into account issues such as patient safety and data security, are being considered.The shared vision for community pharmacy to play an increased role in the delivery of primary care was set out in the 5-year deal. As pharmacy services continue to develop and expand, there is consensus that community pharmacists having the ability to view and contribute to the medical records of patients, where appropriate permissions are given, including but not limited to; access to baseline measurements and pathology results, is necessary to achieve this safely and effectively. Options for additional integration and record access include:
- GP Connect Access Record. This provides direct access to a defined community pharmacist, enabling them to see an appropriate view of a patient’s GP record either as a read-only document, (as an HTML), or subject to further development, and agreement of standards, pharmacists will be able to retrieve structured information from a patient’s GP practice record, see GP Connect – NHS Digital. Further information will be provided regarding this functionality at the Community Pharmacy IT Group (CPITG) meeting on the 8 June.
- Shared Care Records (known as ‘ShCR’, ‘Local health and shared care records’, ‘LHCRs’ or simply ‘records’) include information from multi care settings e.g., General practice and secondary care. National ShCR guidance due out in the summer provides the next steps towards the target for wider implementation of shared care records in 2023/202Engagement and development associated with the Bookings and Referrals Standard (BaRS), the strategic interoperability standard for healthcare IT systems. This will enable booking and referral information to be sent between NHS service providers quickly, safely and in a format that is useful to any clinicians. Working with the BaRS programme we are hoping to prioritise the following use cases; NHS 111 and General Practice to pharmacy (22/23) and secondary care to pharmacy (23/24). An initial workshop has been scheduled for Tuesday 12th July from 10am to 1pm and all system supplier leads would be very welcome to attend. For further information please contact bookingandreferralstandard@nhs.net.
- Payment and Data APIs
The BSA are being commissioned to develop and support application programming interfaces (APIs) for all of the community pharmacy clinical services within the Community Pharmacy Contractual Framework (CPCF). These APIs will support both the payment of service fees along with the provision of additional data to support the future evaluation and commissioning of services. API specifications for COVID and Flu vaccinations, Community Pharmacist Consultation Service (CPCS) and the Smoking Cessation Service (SCS) are already available, and the draft specification for the Discharge Medicines Service (DMS) has just been shared for review. This financial year, the BSA will also develop and issue the API specifications for the Blood Pressure Check Service; the New Medicine Service (NMS) and any future services subject to negotiations. For further information regarding this project please contact rob.hills@nhs.net.
We recognise that this is an incredibly challenging roadmap, and we all want to work with you to ensure this is achievable and will meet the needs of the users, the pharmacy contractors, to provide safe and efficient patient care.
You will have seen that a Prior Information Notice (PIN) was recently issued in relation to CPCF service specific ‘technical toolkits’ that includes references to some or all of the above. Supplier engagement sessions regarding the technical toolkits and feedback opportunities are being scheduled, with further information available from June. In addition, NHSD have also been commissioned to publish a Future Enterprise Architecture document, based on user needs, for community pharmacy covering a number of the foundation services and providing a picture of the longer-term direction of travel. This will be available this summer on the NHSD webpage.
Work is also underway to look into commercial requirements and opportunities that will support both the needs of the sector and system suppliers now and in the future. Further information will be shared in due course. It remains the policy intent that we will continue to support and develop an open supplier market and your views on how we can go about this are always welcome. It is the case that pharmacy contractors, as commercial businesses, cover the costs of their preferred IT solution(s) and have the freedom to choose the supplier that most meets their specific needs.
We are also looking beyond April 2024, working closely with colleagues and stakeholders on the future strategy for community pharmacy and what digital capabilities and requirements MAY be required to support future services. Examples of potential discovery projects include capabilities to support independent prescribing; access to and the recording of pathology and/or phlebotomy tests, additional referral pathways etc. These areas are speculative at this stage, and need to be informed by wider policy developments, such as the Fuller Stocktake and the transition of commissioning to Integrated Care Systems.
We recognise your continued commitment to the community pharmacy sector and the users of your systems, and we share your determination to ensure community pharmacies are able to provide the best possible care within the NHS and have the best IT to be able to do so to support the Community Pharmacy Contractual Framework and beyond.
Our aspirations for this sector remain high and we continue to have an ambitious and challenging roadmap to ensure that pharmacy contractors do have the best IT available to them to support the current 5-year CPCF framework but also the ‘what’s next’.
You will note that we have not mentioned vaccinations within this letter and this is an area where we expect that there may be additional requirements of suppliers providing these services. We are engaging with the vaccination programme and will share more information once this is available.
We trust this letter is received in good faith and look forward to further discussions either via the CPITG or via alternative mechanisms in due course.
Signed on behalf of
NHS England and Improvement (Pharmacy policy team), NHS England and Improvement Transformation Directorate, Department of Health (Pharmacy policy team), NHS Business Services Authority Digital development team and NHS Digital Medicines and PODAC programmes.
IT related to Serious Shortage Protocols (SSPs) and other Drug Tariff reforms
SSPs: SSPs are for use in the event of a serious shortage of a medicine. SSPs give community pharmacies the ability to dispense less, give a different strength or pharmaceutical form, provide an alternative generic product, or provide an alternative product following appropriate discussions with the patient.
The NHS Business Services Authority (NHSBSA) is continuing to identify a significant percentage of SSP claim messages that do not meet the endorsing requirements. That is usually because one or more of the below apply:
- Invalid or incorrect SSP reference number endorsed – For example SSP 000, SSP (missing reference number), SSP 028 (incorrect number), SSP 05 (two instead of three digits).
- Incorrect item endorsed.
- SSP claims for prescribed items without an active SSP.
- Claims for supplies made in accordance with an expired SSP.
Drug Tariff reforms: DHSC has proposed and consulted on reforms to community pharmacy drug reimbursement and previously published its response. The eight proposals relate to changes to:
- the discount deduction scale;
- the way drug prices in non-Part VIIIA are set;
- the way Category A prices are set;
- how medicine margin is distributed in Category M drugs;
- how Category C prices are set for drugs with multiple suppliers;
- the Drug Tariff in relation to inclusion of non-medicinal products within;
- the arrangements for reimbursement and procurement of ‘specials’; and
- the reimbursement of generically prescribed drugs and appliances dispensed as ‘specials’.
System suppliers have fed back that some of these reforms are associated with IT change.
Hormone replacement therapy (HRT): Maria Caulfield, the Conservative MP for Lewes stated that there is an intention for “an annual prescription prepayment certificate (PPC) for HRT items, which is due to be implemented from April 2023. This certificate will allow individuals to access the annual licensed HRT treatments they require for the cost of two single prescription items at £18.70.”
Electronic Prescription Service (EPS)
- NHS Digital EPS and eRD utilisation rate statistics (for the February 2022 dispensing month) are set out on the right.
- NHS Digital’s EPS team are continuing with their assurance work for EPS prescribing and dispensing systems.
- NHS Digital EPS (Next Generation work):
- Discovery and user research taking place around potential for limited prescription tracking for patients using the NHS App.
- Secondary care system suppliers are developing against the prescribing API, and more suppliers are engaged – both prescribing and dispensing systems.
- Development of APIs for dispensing and prescribing system suppliers.
- Prioritisation of technical developments and potential EPS enhancement continues – considering the value/benefits and technical feasibility.
- NHS Digital would like to talk to pharmacy team members about their experience using EPS. User feedback is essential to inform future improvements and the next generation of the system. Please could pharmacy EPS users within the group take part and provide views, by signing up at https://feedback.digital.nhs.uk/jfe/form/SV_eu4jQRNbJooQxoO. This may involve a short telephone interview.
- NHSBSA conducted a survey concerning pharmacy teams’ use of Real Time Exemption Checking (RTEC) during May 2022. The results of this survey will be analysed, and the outcomes will be shared with the CP ITG in due course.
- Community Pharmacy England encouraged pharmacy teams to consider whether Smartcards required renewal. If not renewed, Smartcards expire after two years for information governance reasons. When the renewal date for a Smartcard approaches, the member of the pharmacy team will be prompted to renew every time they login. Community pharmacy team members to check their Smartcards are working regularly and renew them well in advance of their expiry date. Doing so early will mean there is more time to resolve any technical or other issues that may occur during the renewal process. Pharmacy team members can renew their card via the Care Identity Service (CIS) online Smartcard software portal. A large number of Smartcards are due to pass their expiry date in June 2022; 140,000 Smartcards are due for renewal on 27th June 2022. If a Smartcard passes its expiry date without renewal, additional steps will be needed to get the Smartcard working again, therefore, it is advised to renew any Smartcards before their expiry date.
- Community Pharmacy England encouraged pharmacy teams to consider whether Smartcards required renewal. If not renewed, Smartcards expire after two years for information governance reasons. When the renewal date for a Smartcard approaches, the member of the pharmacy team will be prompted to renew every time they login. Community pharmacy team members to check their Smartcards are working regularly and renew them well in advance of their expiry date. Doing so early will mean there is more time to resolve any technical or other issues that may occur during the renewal process. Pharmacy team members can renew their card via the Care Identity Service (CIS) online Smartcard software portal. A large number of Smartcards were due to pass their expiry date in June 2022; 140,000 Smartcards were due for renewal on 27th June 2022. If a Smartcard passes its expiry date without renewal, additional steps will be needed to get the Smartcard working again, therefore, it is advised to renew any Smartcards before their expiry date.
- NHS Digital are documenting the benefits of specific enhancements to support future business cases. NHS Digital have produced 0 of EPS NextGen roadmap, and will welcome further CP ITG input during upcoming workshops.
- The NHS App should receive new messaging capability from December. This will enable discovery work relating to prescription tracking messaging using existing EPS Spine messages, and notifications to patients about EPS status. A CP ITG subgroup will meet with NHS Digital in July 2022 to discuss the proposals.
Real Time Exemption Checking (RTEC)
- NHSBSA has led the RTEC project since January 2020. The CP ITG and Community Pharmacy England have been supportive of its continued roll-out. Read more on RTEC and its phases at: RTEC. Feedback from RTEC users (PSL/EMIS/Cegedim/Titan/Lloyds/RxWeb systems) has continued to be positive.
- The NHSBSA, DWP and the RTEC steering group plan has allowed the expansion of the DWP RTEC functionality to additional pharmacy contractors since the last meeting – from 100 to more than 8,000 sites – a eighty-fold increase. The RTEC team and suppliers have been supporting the ongoing rollout.
NHS App
- The NHS App team are working on further features including:
- Personal Health Records (PHRs) integration with the NHS App.
- Notifications and messages direct to the NHS App: a pilot with 7 GP practices was concluded successfully with positive feedback from citizens, GPs and communication service providers. Messages could include reminders for referral appointments or online consultations.
- NHS account: personalisation. Since April 2022, the project team have given users access to log in to their NHS account direct from the NHS website.
- Access to GP health records. From late 2022, patients with online accounts such as through the NHS App will be able to read new entries in their health record. This applies to patients whose practices use the TPP and EMIS systems.
- NHS Digital has said that analysis supports its view that the NHS App is creating an environmental benefit in reducing the number of care journeys to doctors’ surgeries (this was also reported by Management in Practice).
- NHS App team blogged about developments including progress with the messaging service.
Patient apps and tools
- Gloucestershire CCG is helping thousands test for chronic kidney disease using their smartphones.
- AstraZeneca plans to launch companion apps for patients across different therapeutic areas, including initially asthma, chronic obstructive pulmonary disease and heart failure.
- NHS England announced plans to develop a £240million ‘Federated Data Platform’ (FDP).
- A Trust in Surrey launched a new digital tool for pre-operation assessments, which enables two-way file sharing between the trust and the patient.
- The online Find your NHS Number service was used 4.6million times in its first year.
- Babylon Health selected Google Cloud to join its hybrid-cloud infrastructure.
- The Lancet reviewed ISO standards for health apps.
- A survey suggested 51% of Clinicians Worry That Telehealth Hinders Ability to Show Empathy.
- A new report, Using genomics and drug prescribing identified a number of barriers towards wider adoption of pharmacogenomic tests, including making the most of research evidence, poor availability of tests, health professional education and engagement, and making pharmacogenomic information readily available, for example through electronic systems.
Remote consultations
- NHSE&I published Remote Consultations Guide for Pharmacy. The group fed comments into the guide’s development. Community Pharmacy England along with others also supported its development. Community Pharmacy England has promoted the guidance. Remote consultations have played a critical role during the NHS response to the COVID-19 pandemic. The new guide includes information on:
- the different types of remote consultation;
- when these should be considered as an option;
- how to test and update your processes; and
- how to conduct remote consultations.
IT policy: priorities, reports and the future
- Health Tech Newspaper examined the organisational changes needed within health and care to release benefits from digital technology.
- Digital, Data and Technology Profession (part of the Civil Service) published The digital, data and technology playbook. This looks at an integrated approach to improving technology usage within public services. This includes commercial collaboration, IT structure and resilient cyber security.
- The TEC Action Alliance plans to work with local government, the NHS and integrated care systems, along with umbrella bodies in the disability rights, health, social care and housing sectors, looking at how technology can be harnessed to support the delivery of personalised, affordable and high quality care.
- Dr Pritesh Mistry, Policy Fellow for Digital Technologies at the King’s Fund opined about the present and future of digital tech within NHS.
- Digitalhealth.net published reports:
- A London Trust explained the benefits with trusts using a digital maturity tracking model through the Healthcare Information and Management Systems Society (HIMSS) “a global standard for measuring digital maturity”. Results “scanning your patients, you’re scanning your prescriptions, you’re checking your medication, you’ve got good cyber security – all of that means you are going to deliver better, safer, faster care”.
- The Parliamentary Health and Social Care Committee called for evidence relating to changes with digital technology within the NHS. The inquiry explored the use of technology and examined how it needs to change in order to deliver an improvement in services and outcomes for patients. CP ITG responded to the consultation.
- Ursa Alad (NHSE&I Head of Community Pharmacy Commissioning and MSc candidate, Digital Health Leadership, Imperial College London) is conducting a research project on this topic. The group shared inputs into the study.
IT policy: NHS changes
- Rt Hon Steve Barclay MP has been appointed as the new Secretary of State for Health and Social Care following the resignation of Sajid Javid.
- Simon Bolton has said it is the job of him and his colleagues to ensure that the ongoing merger of NHS Digital, NHSX, Health Education England (HEE) and Innovation, Research, and Life Sciences (IRLS) into NHSE&I is done “with as little impact as possible”.
- Matthew Gould left NHSE&I, the former CEO of NHSX has left NHSE&I.
- NHSE&I chief clinical information officer, Simon Eccles stepped down after four years in the role.
- NHS Digital’s director of research and clinical trials, Michael Chapman, explained about the organisation’s development of a trusted research environment (TRE) in the NHS.
IT policy: global case studies
- Using basic data effectively can improve healthcare and public services. Betanews.com makes the case that the digitization of public services is at the very top of government agendas across Europe, but sometimes the lack of accessible and reliable data, such as core information about organisations and individuals, may create challenges for digital administration.
- European Commission proposal for a Regulation of the European Parliament and of the Council on the European Health Data Space.
- The launch of a proposal on the EU Health Data Space was outlined, this forms the cornerstone of wider European ambitions on digital health and has been prepared during the last few years.
- UK is ‘behind the best countries’ in making all government services digital first, Government Digital Service (GDS) boss admits. They said “The best digital nations in the world have adapted e.g. Singapore, Denmark, Estonia, South Korea, have pivoted and put things mobile first and they have made them hyper personalised for people. We need to really look at these trends: mobile and hyper personalisation.”
- Digitalhealth.net reported that China and the UK are facing similar digital health obstacles and opportunities.
- Medical Economics Journal explored How US digital health was reshaping patient care in USA.
IT policy (general)
- CP ITG published its Pharmacy IT quarterly round-up after the group’s previous meeting.
- CPCS IT contracting arrangements changed from 1st April 2022.
- Community Pharmacy England reported that NHSE&I made Discharge Medicines Service (DMS) funding available to Clinical Commissioning Groups (CCGs). This was so that all acute, community and mental health NHS trusts in England could have the opportunity to support IT solutions or software licenses for DMS.
- The Health and Care Bill became law and included measures which are targeted at supporting data sharing between health and social care.
- The NHS has signed a £25m contract with PA Consulting to support the technology and data systems that underpin national vaccination programmes. Of particular importance is ensuring that IT systems “continue to link national and local booking systems”, according to the contract.
- NHS England and NHS Improvement is asking all Integrated Care Systems (ICSs) to extend or introduce the virtual ward model. Virtual wards have begun to emerge around the country, particularly in Leicester where the University Hospitals of Leicester NHS Trust opened a second virtual COVID ward in February 2021 and became one of the first trusts in the UK to create a virtual ward for patients with atrial fibrillation in March of this year.
- Tomaz Gornik, CEO of Better, explored why we should try to rethink the architecture of health IT in order to unlock the potential of a more patient-centric approach to care.
- A communications technology expert discussed the fragmented processes patients sometimes have to use to contact health care organisations, and potential solutions.
Innovation
- The NHS Innovation Accelerator (NIA) will provide support to 10 innovators so that they can introduce their solutions over the next three years.
- The Amazon Web Services (AWS) Healthcare Accelerator has announced the first 12 innovators who will be joining the UK cohort of its programme.
Inclusion
- Health disparities against minority ethnic groups could increase with AI.
- Putting patients first: championing good practice in combatting digital health inequalities.
Digital capabilities
- A new eLearning programme has been released for health and care staff, to help support the better understanding of the principles of sharing information.
- NHSE&I Transformation Directorate hosted an event to explore what an effective learning network to support digital services should look like for the community pharmacy sector.
- The Organisation for the Review of Care and Health Apps (ORCHA) published a digital health training programme for NHS staff. This has been made available on the NHS learning hub and on the orcha-academy.com
- A study of patients at practices using digital and online tools was published: Access to and delivery of general practice services.
- The NHS Knowledge and Library Hub launched in early 2022.
- Digitalhealth.net published an on-demand webinar: NHS Digital Academy overview.
- NHS Providers blogged about their Digital Boards programme and its successes and failures. The programme is intended to educate boards about technology to reduce the risk of them making ‘bad’ technology decisions.
- NHS Providers has published the fifth part of its Digital Boards programme which looks at how to increase board members’ confidence in delivering digital strategies and to help them avoid common pitfalls.
Development of a Learning network
- As part of its work to develop a pharmacy digital strategy, the NHS Transformation Directorate has been tasked with exploring options to develop a ‘National Community Pharmacy Learning Network’, whereby best practice and ideas can be shared. The learning network was one of the items identified during the Kaleidoscope engagement workshops about digital strategy held last year, and which many CP ITG representatives attended. The NHS Transformation Directorate has commissioned Kaleidoscope Health and Care to assist with this learning network discovery work: The discovery team are considering:
- What would a successful learning network look like for you?
- What gaps currently exist in sharing learning and best practice between different Pharmacy stakeholders?
- What are the disadvantages with learning networks?
- What sort of topics would you like to discuss in a network like this?
- What would make the learning network as engaging as possible for you?
- How can we ensure a learning network is sustainable?
- Pharmacy team members may feed back to it@cpe.org.uk with views on these questions or register to attend a Learning Network workshop on the 17th March 2021 (10.00-11.30am) hosted by NHS Transformation Directorate. CP ITG pharmacy representatives will also be invited.
IT policy: priorities and reports
- NHSE&I announced its 2022/23 digital priorities in wider planning guidance. Healthcare IT News reported on the priorities.
- Group of Seven (G7) (the inter-governmental political forum) working groups produced international reports on: access to health records; digital health progress; standards and interoperability.
- The House of Commons Committee of Public Accounts highlighted challenges with implementing large scale government digital programmes: “Ministers generally spend a relatively short time in any one post, while Permanent Secretaries typically only serve five-year terms. Neither is likely to remain in post for the entire duration of a major digital change programme. Digital change planning therefore needs to be a core activity for Whitehall to deliver as “business as usual”, as some programmes could take up to 20 years to deliver fully.” The Committee have made a series recommendations.
- NHSX published its review of adult social care technology and digital skills.
- DHSC published the People at the Heart of Care: adult social care reform white paper which sets out a 10-year vision for adult social care and provides information on funded proposals to be implemented by 2025.
- Digital healthcare leaders reacted to NHS IT funding pledges.
- Chief Technology Officer, Mark Reynolds, highlighted the sustainability challenges facing the digital sector and explored how NHS Digital plans to tackle them.
- Public Accounts Committee’s report published a paper: Challenges in implementing digital change.net reported that reported on the topic.
- The HSJ reported that NHSE&I has launched review into digital tools in primary care (login/subscription required).
- The House of Commons Health and Social Care Committee recommended “NHSE&I publishes its evaluation of digital tools in primary care at the earliest opportunity and uses it to produce clear guidance on best practice in reducing bureaucracy and day-to-day IT administration tasks, including those associated with referrals, and follow-up appointments.”
- A European case study set out how five European countries effectively used technology and Shared Care Record systems before and during the pandemic.
Events and digital development
- An upcoming webinar will be held on accelerating Shared Care Records (ShCR) and related IT standards. It will be held on Monday 21st March 12:00-14:00 and hosted by the Professional Record Standards Body (PRSB). Pharmacy team members with an interest with ShCR are encouraged to register to attend.
- NHS Digital Health Leadership Programme is open to applicants until 24th March for the next cohort of digital leaders (learning begins September). Pharmacy and other applicants can find out more about the application process at the NHS Digital Academy application webpage and the rest of the NHS DA website.
IT policy: NHS organisational changes
- Wade-Gery’s review Putting data, digital and tech at the heart of transforming the NHS was published with its focus on progressing technology within the NHS by having the having the right capabilities and set up at NHSEI, NHSX and NHS Digital.
- DHSC announced that NHS Digital, NHSX and Health Education England will be absorbed into NHS England and NHS Improvement (NHSE&I) as part of plans to develop the workforce and improve technology across the NHS in England. This followed the Wade-Gery review into digital within NHS including co-working amongst the NHS bodies. NHSX has become the NHS Transformation Directorate digital strategy directorate within NHSE&I, and NHS Digital will become the Chief Information Officer’s directorate within NHSE&I. NHSX and NHS Digital branding is anticipated to eventually be phased out. NHSX blogged about the changes.
IT policy (general)
- An industry insider opined on the, future regulatory landscape will look like within digital health.
- Health tech suppliers made predictions about the rest of 2022.
- Health & Social Care Committee urged the government to ‘further progress’ NHS digitalisation.
- New data showed patient–led digital adoption from the start of the pandemic is being sustained.
- A recent case study indicated continued demand for digital appointments: 89% of NHS Trusts had delivered new digital appointment services as a direct response to the Covid-19 pandemic and the remaining 11% already had digital appointment services in place and further expanded their use. A YouGov survey of GB adults (18+) showed that 48% prefer digital communications for healthcare providers, which increases to 69% if you include telephone communications.
- Research indicated the lack of digital skills in NHS staff could be slowing the rate of digital transformation in the health system.
- NHS Providers published a guide aimed at trust boards about ‘Making The Right Technology Decisions’ as part of the Digital Boards Programme.
- CP ITG published its Pharmacy IT quarterly round–up after the group’s previous meeting.
Innovation
- A King’s Fund policy leader made a case for the importance of culture and leadership to drive forward digital innovation within the NHS.
- The DigitalHealth London Accelerator programme welcomed 21 digital health companies.
- NHSX’s Digital Productivity Programme is using evidence–based research to identify the greatest benefit–realising digital technologies g. in chronic wound management – where without removing the bandage an electronic ‘tag’ can provide doctors with vital information about how a wound is healing.
Intro to NHS Booking and Referral Standards (BaRS)
- NHS Digital’s Booking and Referral Standard (BaRS) team aims to enable booking and referral information to be sent between NHS service providers in a format useful to clinicians. The intentions are that it will eventually be available in all care settings. Pharmacy use cases are currently being considered including the potential for referrals from 111 to community pharmacy.
- NHSE&I is developing a standards roadmap to go live in April 2022 which will provide a list of proposed and developing data, information and technical standards, including potential changes to existing standards. BaRS is listed as a major priority.
- The BaRS team provided an update at the CP ITG Spring 2022 meeting.
NHS Profile Manager
- Currently, community pharmacy contractors use two different NHS systems to ensure their pharmacy details are up to date in the Directory of Services (DoS) and on the NHS website: the NHS website profile editor and the DoS profile updater.
- A new tool, NHS Profile Manager is scheduled to replace both the DoS Updater and the NHS website editor in spring 2022. During late 2021 and early 2022, NHS Digital reviewed all the existing users of the NHS website profile editor and any users who are not using an email address ending with nhs.net received email instructions on how to update their login details.
- A CP ITG sub group attended two demo meetings, both of which have been recorded and posted online: CP ITG Profile Manager Demo and meeting video 1 (December 2021); and Demo and meeting video 2 (February 2022). The group also discussed future enhancements with NHS Profile Manager team.
- In February, Community Pharmacy England published communications about progress with the launch and further communications will be published in due course about the release plan. The group are encouraged to support the cascade of messages.
- Multiples head office staff needing to use NHS Profile Manager should create a personal NHSmail account if they have not already done so. Advice is at the ‘NHSmail personal accounts: creation and linking’ section of Community Pharmacy England’s NHSmail
- NHS Digital will also be working with pharmacy multiples regarding the NHS website and DoS Application programming interface (API).
Shared Care Records (ShCR) update
LPCs and/or local contractors can continue to take steps to gain pharmacy access such as:
- identifying the ShCR project team from the List of records systems (recently updated);
- learning about case studies such as Dorset Care Record ShCR pharmacy access case study and the East London Patient Record (eLPR) pharmacy case study;
- contacting the ShCR project team and other local partners to find out how to get involved;
- using the ‘Planning pharmacy access briefing’ and frequently updated ShCRs webpage; and
- reviewing the previous Community Pharmacy England/RPS ShCRs/SCR letter to NHS orgs about records access.
Community Pharmacy England continues to work with NHS Transformation Directorate and other relevant stakeholders on the actions set out within the Shared Care Record (ShCR/LHCR) NHS and pharmacy outputs document. Local Pharmaceutical Committees (LPCs), ShCR project teams and other parties supporting ShCR pharmacy deployment are encouraged to contact it@cpe.org.uk with technical ShCR information so that supplier and IT support helpdesks can whitelist several ShCR domains at the same time.
Records
- NHS Digital supported by Community Pharmacy England carried out user research into pharmacy preferences about the Summary Care Record (SCR) Alert Viewer to inform some adjustments to the tool.
- The BMJ explored the barriers and challenges to better access to personal health records.
- BMA expressed concerns about timing for NHS App patient record access rollout.
- Digitalhealth.net published a special report on ShCR and ICS progress.
- The Greater Manchester Care Record has begun receiving information from an app used by local care home staff for Covid management.
Standards and interoperability
- NHSE&I is developing a standards roadmap to go live in April 2022 which will provide a list of proposed and developing data, information and technical standards, including potential changes to existing standards. BaRS is listed as a major priority. NHS Transformation Directorate are seeking feedback on the roadmap structure and content. If you think there is anything missing from their standards roadmap list, or you have a query the Standards & Interoperability team can be reached at: interop.standards@nhsx.nhs.uk.
- NHS Digital published an Information Standard to support improved medication and allergy/intolerance information sharing across healthcare services in England. It does not currently apply to EPS but could relate to pharmacy services IT.
- NHS Digital blogged about their API sunsetting process.
- net published a special report about how the Medicines and Healthcare products Regulatory Agency (MHRA) would help improve interoperability nationally and internationally.
- At a previous meeting, the group agreed to support the capability for anonymised data to be accessible, so that pharmacy teams’ interventions can start to be auditable, and the value of community pharmacy can be better demonstrated. If PMR systems were to be adapted to allow such data sharing, it would require the development of a roadmap and a standard approach to data provision, which may benefit from use of SNOMED CT clinical terms. A PSNC-drafted dataset was prepared and a dataset for the Community Pharmacist Consultation Service (CPCS) could be added. If you would like to help with this work, please contact it@cpe.org.uk.
Standards case study
- Case study: How NHS Digital used API Management to support APIs at scale. NHS Digital implemented an API management platform to help them roll out digital healthcare services more quickly and consistently. The team at NHS Digital set an API management vision with goals to make it easier for suppliers engaged with the project team to: o onboard, by only asking developers to do things that are needed; o learn, by making documentation available online;o design and build, by making APIs internet-facing and using open standards; o test, by providing developers with sandbox environments for early and easy testing; and o get help and support with self-serve support and reliable help resources.NHS Digital has bronze, silver, gold and platinum service classifications. Early in the project, the API was initially classified as a bronze service which meant, among other things, support was limited to within office hours. The team switched to platinum and were able to offer a rolling out 24-hour support. The team set up an on-call rota; the rota makes sure someone is available to respond to emergencies and provide backup support. The outcomes of the project were improved lead time, improved supplier rating and engagement.
NHSmail updates
- NHSmail support pages outline the benefits of the NHSmail Teams “Virtual Visits” patient consultation platform – namely, this platform enables appointment booking and video consultation. The NHSmail team previously provided a demo of the tool to Community Pharmacy England and CP ITG representatives. Several contractors amongst the small alpha pilot group have now begun to successfully use and pilot Virtual Visits.
- Pharmacy contractors within the group who are not already participating in the pilot are encouraged to take part by completing the volunteer form. The second round of (beta) piloting is due to start from early March 2022.
- The group will be asked to provide feedback about the Virtual Visits email address naming convention: e.g. for MediGood a recommended format such as:
- nhspharmacy.MediGood.ODScode.appointments@nhs.net and display name “MediGood (NHS Pharmacy)”.
- The NHSmail team will be stopping the hard-copy postal one-time passcode (OTP) option currently used to authenticate new users registering for NHSmail, a paperless method is scheduled to be used from late March 2021.
- Community Pharmacy England communicated NHSmail Teams guidance.
- Survey results suggested Microsoft Teams is helping many health and care staff save time.
Virtual Visits: How it works
The Virtual Visits tool provides pharmacy contractors with an appointments system so that pharmacy teams can notify patients and better manage appointments. Pharmacy teams can also use the Virtual Visits tool to conduct face to face or virtual patient consultations (audio or video). The tool works in conjunction with NHSmail Microsoft Teams and the Microsoft Booking platform. To participate in the pilot, you must have: an active personal NHSmail account; access to a shared NHSmail inbox; MS Teams installed on a computer or tablet; and a computer or device with a webcam.
Data Security and Protection Toolkit (DSPTK)
- Community Pharmacy England and NHS Digital are currently updating the Data Security and Protection Toolkit (DSPTK) and related tips. Additional user testing is also planned. If you would like to get involved with this user testing, please contact it@cpe.org.uk.
- NHS Digital may update contractors about the availability of the initial Toolkit version. However, we strongly recommend that contractors hold off accessing the Toolkit until the planned improvements have been finalised and Community Pharmacy England releases its updated guidance. Contractors will still have adequate time to complete the Toolkit before the submission deadline on 30th June 2022. We will keep contractors informed of any developments.
Other data security updates
- NHS Digital published a feature about how ransomware can affect organisations and what is being done to combat it. “On 14th May 2021, the IT systems of the Health Service Executive (HSE), (Ireland’s equivalent of the NHS), were hit by a cyberattack. The perpetrators, suspected to be a Russian-based criminal gang, had used software to infiltrate systems.”
- Cyber expert guidance was issued about how far cloud adoption can help the NHS.
- Microsoft announced Windows 11 plans. Many Windows 10 users are currently eligible for a free upgrade to Windows 11, provided that the computer meets the strict minimum system requirements (e.g. 64-bit processor and 4GB RAM). Pharmacy contractors are advised not to update their machines without the agreement of or supervision from their IT support. Read more: CP ITG: Windows briefing.
- NHS website crashed when many tried to book Covid booster jabs during December 2021
- NHS Digital previously added the multi-site ‘FFFFF’ Smartcard code and SCR rights onto Smartcards with the pharmacist or pharmacy technician role, because of the COVID-19 pandemic. The initiative was supported by Community Pharmacy England and NHS England and NHS Improvement. NHS Digital previously confirmed to Community Pharmacy England that assignment codes are further extended until 31st March 2022.
Paperless
- The group previously identified going paperless as a priority – within its Digital Priority List and Views on the next generation of EPS However, pharmacy teams continue to report considerable use of paper and printing for reasons such as enabling prescription information to move around the dispensary given limited space for PMR terminals. Following work with the group and the paperless sub-group the ‘Going paperless’ webpage is now available.
- For the April 2022 dispensing month onwards the NHSBSA Manage Your Service (MYS) system will be the route for monthly FP34C submissions instead of the legacy paper submission method.
- NHS Digital published its Annual Sustainability report including case studies highlighting the system-wide environmental impacts of some of its 2020-21 technological interventions such as provision of NHS App.
- Eight executives opined about whether hospitals could go ‘too digital’?.
Data
- NHS Digital Organisation Data Service (ODS) team has launched the new ODS DataPoint service enabling you to quickly download customised reports relating to ODS and pharmacy data.
- NHSX, NHS Digital, Community Pharmacy England and others are supporting an initiative to rationalise central lists of pharmacy data used within NHS systems and datasets. This will help align data, reduce pharmacy workload, and improve accuracy and data quality. The workstream is also helping to identify future NHS Profile Manager enhancements, some of which are being added to the roadmap.
- The NHS Digital Terminology Server now includes data from the NHS Dictionary of Medicines and Devices (dm+d), through the Terminology Server’s web API. The old method of downloading XML files from the Technology Reference Update Distribution (TRUD) is still available. NHS Digital plan to add Global Trade Item Numbers (GTINs, the numbers used on barcodes) and information about ingredient strength for multi-ingredient products in April 2022.
CPCS IT
- NHSE &I and Community Pharmacy England previously announced that a national procurement model would be in place to support community pharmacy contractors with the delivery of the Community Pharmacist Consultation Service (CPCS). This was originally scheduled to end on 1st October 2021 but was extended to the end of March 2022. Given that the contractual arrangements from 1st April 2022 will be solely between the supplier and pharmacy contractor, contractors should make the necessary preparations as soon as possible. Contractors need to consider their choice of CPCS IT supplier and either confirm to their existing supplier that they will be staying with them or inform a new supplier that they will be using their system. Contractors will be able to transition to their own contractual arrangements with one of the four assured IT providers[1]: Cegedim; Positive Solutions; Sonar Informatics; or PharmOutcomes. NHSE&I and NHSX published the CPCS IT Provider ‘Switching’ guide and the CPCS IT Buyer’s Guide with inputs from partner organisations including Community Pharmacy England.
- Contractors are encouraged to make their decisions well in advance of the upcoming deadline. Group members are asked to communicate on this topic to their networks and can use the CP ITG CPCS IT communications copy and future Community Pharmacy England and NHSE&I bulletin news items.
Recommended minimum transfer dataset for pharmacies switching from one patient medication record (PMR) system to another
- The group previously supported developing a recommended minimum dataset for cases where a pharmacy contractor has switched from one PMR system to another. A previous draft iteration was supported by the group. For the sake of continuity of patient care, it is critical for some patient information to be transferred from the old to the new system.
- A drafted dataset has been prepared incorporating the comments from previous group meetings and suppliers. An associated specification document has also been prepared. The dataset is not comprehensive for all those records within pharmacy systems, but the dataset is intended to be a starting point as a means to strengthening the data quality. Suppliers recently requested changes, including:o arranging the data into tables instead of within a data block (via JavaScript Object Notation (JSON) format); and o categorising the data by Medicines, Patient, Prescriber and Prescribing Organisation.
- Suppliers are asked to send comments to it@cpe.org.uk by the end of March 2021.
- The secretariat will arrange a joint call with suppliers to talk through the updated dataset.
Supplier letter
System supplier previously fed back that multiple projects were ongoing or forthcoming within the NHS (see: Appendix CPITG 03A/06/21 Gantt Chart (slide) and spreadsheet version). A group of system suppliers prepared a letter addressed to NHSE&I, the Department of Health and Social Care (DHSC) and other pharmacy IT policy makers to explain the benefit of advance IT project planning. The letter explains “We do not wish to delay or prevent innovation and change. We welcome changes which benefit pharmacies, their patients and the NHS. However, we would welcome a deep consideration about how policy makers can ensure that IT system providers in the pharmacy sector are provided with adequate notice ahead of changes being made to ensure the best possible running of pharmacy IT systems and changes.” The letter also proposes enhanced NHS IT assurance processes; that suppliers should be able to collaboratively feed into NHS IT specifications throughout the course of their development; and that suppliers should be able to submit information about their company and solutions to the NHS once.
- The group previously published its “Use and development of pharmacy systems – Suggested features list v1.0”. Additional feedback has led to this document being significantly updated. Suppliers and the group are encouraged to share final comments, by emailing it@cpe.org.uk during March 2022. The updated list will be published shortly after the March 2022 meeting. See: “CP ITG– Use and development of pharmacy systems – Suggested features – comments.docx.
- NHS Digital EPS and eRD utilisation rate statistics (for the November 2021 dispensing month) are set out on the right. o NHS Digital’s ESP team are continuing with their assurance work for EPS prescribing and dispensing systems for current and Next Gen EPS.
- NHS Digital EPS (Next Generation work):
- Secondary care system suppliers are developing against the prescribing API, and more suppliers are engaged – both prescribing and dispensing systems.
- Development of APIs for dispensing and prescribing system suppliers.
- Discovery work is ongoing around use of EPS for secondary care outpatients to homecare.
Prioritisation of technical developments and potential EPS enhancements continues – considering the value/benefits and technical feasibility.
- NHSE&I, NHS Digital, and the CP ITG discussed developments at the CP ITG March meeting.
Real Time Exemption Checking (RTEC)
- NHSBSA has led the RTEC project since January 2020. CP ITG and Community Pharmacy England have been supportive of its continued roll-out. Read more on RTEC, its phases at: RTEC. Feedback from RTEC users (PSL/EMIS/Cegedim/Titan/Lloyds/RxWeb systems) has continued to be positive.
- NHSBSA, DWP and the RTEC steering group plan have allowed the expansion of the DWP RTEC functionality to additional pharmacy contractors since the last meeting from fifty to 100 sites.
- The NHS Business Services Authority (NHSBSA) said that Real Time Exemption Checking (RTEC) had performed 100 million checks.
NHS Digital seeking pharmacy user research volunteers to support digitising the Valproate form
- The Valproate Annual Risk Acknowledgement Form (ARAF) helps to confirm the necessary Pregnancy Prevention Programme (PPP)[1] for those patients being prescribed sodium valproate. A specialist completes the ARAF with the patient and the ARAF information goes back to the GP practice usually by post. NHS Digital are doing discovery work about: How to digitise the form? o Which parts of the form might digitally flow into the GP practice system? What bits of information in the form are the most relevant to pharmacy professionals?
- NHS Digital are seeking pharmacy user research participants to look at the ARAF and comment about which bits seem the most relevant and why. The research is expected to be undertaken via polls and 15-minute interviews. Some of the work is anticipated to begin during the second half of 2022 which allows a period of discovery before this. Contractors that wish to take part may contact it@cpe.org.uk. Community Pharmacy England will forward volunteers’ details to the project team. CP ITG has also signposted the project team to the Community Pharmacy Patient Safety Group (CPPSG).
NHS App
- NHS App reached more than 22 million users by end of 2021 with over 16 million new users since the COVID-19 vaccination status service was added in May 2021. The NHS App is available on the Google Play store and the Apple App store. More than 28 million people have registered with NHS login – over half of the English population.
- The NHS App team are working on further features including:
- Personal Health Records (PHRs) integration with NHS App. o Notifications and messages direct to the NHS App: being piloted in 7 GP practices as of February 2022. Messages include reminders for appointments or online consultations. o NHS account: personalisation. Since January 2022 NHS App team have been trialling updated service journeys on NHS website and are exploring how to enable users to easily update their account contact details.
- Access to GP health records. From April 2022, patients with online accounts such as through the NHS App will be able to read new entries in their health record. This applies to patients whose practices use TPP and EMIS systems. PulseToday reported on progress.
- NHS App team blogged their work enhancing the patient messages features to better satisfy the growing appetite of users to receive their communications digitally.
- NHS Login is now being hosted on Amazon’s AWS cloud service.
Apps and tools
- NHS Transformation Directorate offered thousands of blood pressure monitors to patients to monitor their BP at home and send readings to their GP via phone, email or digital platforms.
- The government is piloting an anti–obesity app.
- The Lancet analysed GP consultation methods and amongst its findings were: face-to-face appointments in England decreased from 9m in February, 2020, to 3m in two months later, they have since increased by 90% (5m in August, 2021). Simultaneously, telephone consultations trebled during this period (from 2m in February, 2020, to 6m 18 months later). The growth in remote consultations has seemingly allowed for a substantial increase in the number of overall consultations, compared with pre-pandemic levels.
Artificial intelligence (AI) and robotics
- Microsoft and Babylon Health are co–working to improve accessibility of healthcare worldwide.
- Office for Artificial Intelligence (OAI) plans to set out a national approach for AI regulation.
- The Alan Turing Institute was selected to lead on the piloting of a new AI Standards Hub.
IT policy updates
Integrated Care Systems (ICS)
- Community Pharmacy England published a one-page ICS and healthcare IT factsheet.
- Integrated Care Systems will be required to have digital and data platforms in place by April 2022.
- The requirement for all of England to be covered by an Integrated Care System (ICS) was introduced to parliament.
IT policy: lessons from the pandemic
- A more “systematic” approach to data collection and sharing is needed to better prepare for future pandemics, according to a report from the G7 summit.
- Richard McEwan, Lead Technical Architect, explains the infrastructure behind one of the world’s largest national COVID-19 vaccination programmes and how it has helped over 35 million people and counting get their life-saving jabs.
- A new study has revealed the majority of the UK’s leading health providers are accelerating their digital transformation plans this year in response to the Covid pandemic.
- NHS Digital received an award for statistical work to identify those patients most vulnerable to COVID-19 so that their care was prioritised. NHS Digital’s Chief Technology Officer considered How data shielded the vulnerable.
IT policy: changes to the landscape
- Digital Health Network’s Advisory Panels elected new members.
- Tributes were paid to NHS Digital’s deputy CEO Pete Rose also serving as the organisation’s chief information security officer (CISO) who passed away in August 2021.
- Digital Health reported on Amanda Pritchard’s appointment as NHS England’s new CEO.
- New interim chief executive of NHS Digital Simon Bolton outlines his main priorities including to further improve working relationships between NHS England, NHSX and NHSD.
- Digital Health opined on the biggest tech challenges for health secretary Sajid Javid.
CP ITG IT infrastructure survey
- Contractors and others can promote the newly launched survey using template wording. Please can pharmacy contractors and teams also submit an IT arrangements survey response within October. The results will help inform IT policy of system suppliers and the organisations which attend CP ITG.
dm+d code changes and synchronisations
- Community Pharmacy England received system supplier and pharmacy contractor feedback about changes to dm+d codes impacting on the use of EPS.
- Pharmacy contractors should report actual or potential clinical impacts using the Learn from patient safety events (LFPSE) process outlined at the dm+d webpage reporting guidance section.
- NHSBSA dm+d team are reviewing their scope to provide notifications ahead of changes and have already started to introduce some communications earlier than usual via the Technology Reference data Update Distribution communications route.
- Supplier comments have proposed that if dispensing and prescribing systems targeted aligned synchronisation dates this would reduce the risk that pharmacy contractors received problem prescriptions for items which have had changed dm+d entries. However, there are challenges given that some prescribing suppliers reportedly synchronise less often compared to pharmacy system suppliers and additionally whilst the drugs database update may be made available monthly for prescribers, it may take two to three weeks after the update for it to reach all GP practices using that system. Pharmacy system suppliers will contact the CP ITG secretariat within October 2021.
IT policy key updates
- Community Pharmacy England published a one-page ‘Reshaping how health and care data is used’ factsheet about DHSC proposals in their Data saves lives paper.
- World Health Organisation (WHO) forecasts global 13 million shortfall of health workers by 2035.
- Medical Futurist reports on Google’s plans in the health and care sector.
- Kings Fund published a long read about the impact of NHS administration processes on patients.
- NHS Digital calculated a digital revolution in social care might have £127m in future benefits.
- King’s Fund considered the journey towards a smarter hospital within an integrated landscape.
- Hospitals expected to begin testing electronic prescribing systems from autumn 2021.
- CP ITG published its previous Pharmacy IT quarterly round-up after the last CP ITG meeting.
- Microsoft announced Windows 11 plans.
- BT say Public Switched Telephone Network (PSTN) phonelines will all be disconnected within four years. Pharmacy contractors will need to ensure they connect their phones into an internet connection (Voice Over Internet Protocol (VOIP)) and consider contingencies if internet is lost.
Innovation
- Digital Health London launched Innovation Directory for London to help accelerate digital change.
- An openaccessgovernment.org opinion piece argued that innovation can resolve NHS challenges.
- AHSN Network published an innovation in healthcare study.
- NICE and AHSN have announced a two-year agreement to support the use and promotion of innovation in the NHS.
Digital capabilities
- Health Education England selects new consortium to deliver NHS Digital Academy programme.
- Health Education England published a Digital Capabilities in the Pharmacy Workforce
- UK Parliament reported on the extend of digital literacy amongst citizens. Data suggests around a fifth of the population do not have “essential digital skills” for life as defined by the UK Government – impacting their ability to access services, get employment and healthcare.
- The US core pharmacist curriculum has had additional Genomics content added.
Inclusion
- Local Government Association (LGA) has launched a Digital Pathfinders Programme with a promise of support of up to £20,000 each for a number of projects led by local authorities aiming to improving digital inclusion, connectivity in their communities and cyber security.
- NHSX and others published a factsheet for digital project teams to consider digital inclusion as part of their work.
- NHSX plans to further develop an NHS Account to simplify patient access to digital services.
- Emma Stone, Director of Design, Research and Communications at the Good Things Foundation, explored the implications of increased use of digital health services on the digital divide.
Healthwatch reported on how some patients had been excluded by remote GP appointments
Interoperability and records
Shared Care Records (ShCR) update
Updates about ShCR arrangements have been included within previous meeting papers and discussed at past meetings. ShCRs were previously called ‘Local health and shared care records (LHCRs)’.
LPCs and/or local contractors can continue to take steps to gain pharmacy access such as:
- identifying the ShCR project team from the List of records systems;
- learning about case studies such as: Dorset Care Record ShCR pharmacy access case study and the recently published East London Patient Record (eLPR) pharmacy case study.
- contacting the ShCR project team and other local partners to find out how to get involved;
- using the ‘Planning pharmacy access briefing’ and frequently updated ShCRs webpage; and
- reviewing the December 2020 Community Pharmacy England/RPS ShCRs/SCR letter to NHS orgs about records access.
CP ITG pharmacy reps and LPCs took part in the Virtual ShCRs event (1st July 2021). Community Pharmacy England continues to work with NHSX and other relevant stakeholders on the actions decided at this meeting. More information about these actions is available here: minutes and outputs for the Shared Care Record (ShCR/LHCR) summer 2021 event.
Records
- NHS Digital launched a Data Uses Register tool so patients can see which organisations access certain data (also reported by Digital Health).
- NHSX is looking at how new IT could allow pharmacy teams to add notes to patient records.
- NHSX launched procurement framework for digital social care records.
- NHS England and NHSX plan to invest £52 million into online maternity records.
- Royal Marsden Hospital announced a partnership with Great Ormond Street Hospital to deliver a new digital health record powered by the supplier, Epic.
- Clinical and system leaders from Greater Manchester presented a virtual September 2021 event about the progress with use of the ShCR ‘Greater Manchester Care Record’.
- Genetic test results for urgent cancer patients can now be accessed digitally across Wales.
- North Tees and Hartlepool Hospital integrated into the Great North Care Record.
- A case study explored how to manage healthcare data volumes in health care records (e.g. more high-resolution images).
Other updates about interoperability
- Enovacom launched a FHIR: everything you need to know (short factsheet) about Fast Healthcare Interoperability Resources.
- The Royal Wolverhampton NHS Trust has extended its partnership with Babylon.
- NHSX Blueprinting Steering Committee said that Blueprints are important for delivery of digital capabilities within the NHS. The committee considers blueprints a knowledge asset and a product of a structured approach to learning, from projects that have taken place. The committee is overseeing the development of hundreds of new blueprints.
- NHS Digital announced the first providers had begun taking part in the national data alignment programme between the NHS and private sector.
- At a previous meeting, CP ITG agreed to support the capability for anonymised data to be accessible, so that pharmacy teams’ interventions can start to be auditable, and the value of community pharmacy can be better demonstrated. If PMR systems were to be adapted to allow such data sharing, it would require the development of a roadmap and a standard approach to data provision, which may benefit from use of SNOMED CT clinical terms. A PSNC-drafted dataset was prepared and a dataset for the Community Pharmacist Consultation Service (CPCS) could be added. If you would like to help progress this work, please contact it@cpe.org.uk.
NHSmail
NHSmail support pages outline the benefit of the NHSmail Teams “Virtual Visits” patient consultation platform – namely, this platform enables appointment booking and video consultation. The NHSmail team provided a demo to Community Pharmacy England and CP ITG representatives. Pharmacy contractors that would like to pilot this can contact it@cpe.org.uk with their name, ODS code and telephone number and ‘Virtual Visits pilot’ within the email subject title.
IG, identity and security
Data Security and Protection Toolkit (DSPTK)
- Community Pharmacy England and NHS Digital are currently updating the Data Security and Protection Toolkit (DSPTK) and related tips. Additional user testing is also planned. If you would like to get involved with this user testing, please contact it@cpe.org.uk.
- NHS Digital may update contractors about the availability of the initial Toolkit version. However, we strongly recommend that contractors hold off accessing the Toolkit until the planned improvements have been finalised and Community Pharmacy England releases its updated guidance. Contractors will still have adequate time to complete the Toolkit before the submission deadline on 30th June 2022. We will keep contractors informed of any developments.
Data security key updates
- Community Pharmacy England and NHSX published a joint Cyber security tips IT factsheet for pharmacy teams.
- The implementation date of September 1st 2021 of the GP Data for Planning and Research (GPDPR) programme was The proposed changes will apply only once criteria is met.
- World Health Organization published a report to help national health systems protect data.
- The Irish government confirmed it was aware that health data could have been stolen during a major cyber-attack and that data may potentially may be abused by criminals. Davey Winder, cyber security expert gave his thoughts on the Irish incident.
- Moorfields Eye Hospital in Dubai was subject to an IT security incident.
Promoting good IT, and user research opportunity
NHS Service Finder enhancements and user research
- NHS Service Finder is a free tool that provides access to information from the Directory of Services (DoS) and the NHS website. It is not accessible by the public, but it does allow pharmacy teams and other healthcare professionals to search for service information quickly. The NHS Service Finder team published user survey results in August 2021.
- NHS Digital user researchers are conducting a further round of user interviews to help further develop the NHS Service Finder tool. If you’d like to take part email it@cpe.org.uk.
Discovery work about patient digital authentication
- Discovery work about patient digital authentication: Community Pharmacy England and CP ITG are feeding into DHSC who are carrying out related discovery work and must explore: the best way to capture digital authentication in community pharmacies; main challenges in implementing digital authentication; and main benefits in implementing digital authentication (for pharmacies/patients).
- Contractors may submit further information into a survey at: https://forms.office.com/r/VYUw5geidT by 20th October 2021. CP ITG and Community Pharmacy England will collate further feedback such as via survey and will share the output to DHSC.
Key reducing burden updates
- CP ITG previously identified going paperless as a priority – within its Digital Priority List and Views on the next generation of EPS However, pharmacy teams continue to report considerable use of paper and printing for reasons such as enabling prescription information to move around the dispensary given limited space for PMR terminals. Following work with CP ITG and the paperless sub-group the ‘Going paperless’ webpage has been further updated.
- More than half of contractors were using MYS for end-of-month submission by August 2021.
- The Government temporarily suspended the requirement for patients (or their representatives) to sign the back of NHS prescription forms or EPS tokens from 1st November 2020 until 30th August 2021. Community Pharmacy England reported on the end of this temporary suspension.
- Community Pharmacy England published a factsheet that explains how pharmacy team members can check if they have an older NHS Smartcard needing replacement in case it is reaching ‘end-of life’ this calendar year.
- NHS Digital previously added the multi-site ‘FFFFF’ Smartcard code and SCR rights onto Smartcards with the pharmacist or pharmacy technician role, because of the COVID-19 pandemic. The initiative was supported by Community Pharmacy England and NHS England and NHS Improvement. NHS Digital have confirmed to Community Pharmacy England that assignment codes will be further extended until 31st March 2022.
- Medical Futurist explored how Drones may be used to support the delivery of health and care.
Development of pharmacy systems
Use of pharmacy systems for CPCF services
- DMS was introduced as an Essential service in early 2021. NHSE&I and Community Pharmacy England were keen for suppliers to be given information on the service, IT implications and dataset requirements. Supplier briefings occurred in October 2020, February and May 2021. Contact persons on the project introduced themselves to CP ITG There is an objective to progress the specification work further during autumn, and for a ‘go-live date’ ideally by late 2021. Community Pharmacy England is continuing to push for this work to be completed at the earliest opportunity. Updates will be published at: cpe.org.uk/itrequirements and cpe.org.uk/dms.
- NHSE&I announced that a national procurement model would be in place to support community pharmacy contractors with the delivery of the Community Pharmacist Consultation Service (CPCS). This was scheduled to terminate on 1st October 2021, but was extended to the end of March 2022. Contractors are recommended to start considering which CPCS IT supplier they want to choose well in advance of the next change. From the autumn, contractors will be able to transition to their own contractual arrangements with one of the four assured IT providers: Cegedim; Positive Solutions; Sonar Informatics; or PharmOutcomes.
- NHSE&I has published a CPCS IT Provider ‘Switching’ guide and additional buyers guidance and an NHSE&I CPCS IT webinar is expected shortly on Thursday 14th October, from 7.00-8.30pm.
EPS and RTEC
EPS
- Since the last meeting, Community Pharmacy England has restructured and revised the webpages within its EPS website section. Community Pharmacy England has also updated its EPS totals reconciliation guidance (EPS totals) guidance and reported on EPS script volumes exceeding 95% of total items.
- EPS Serious Shortage Protocols (SSPs): The current ‘NCSO workaround’ is being phased out and it is recommended that all contractors and system suppliers ensure they are using the EPS SSP endorsement instead of NCSO as soon as possible. NHSBSA is issuing some guidance and support to system suppliers implementing the EPS SSP feature. Suppliers also have some flexibility as to the extent to which they will support pharmacy team members for example, by asking users to complete any missing or incomplete SSP endorsement information if the required endorsements are not present or not in the specified format. NHSBSA has received examples of invalid/incorrectly endorsed SSP claims submitted via EPS. Community Pharmacy England tips explain how to avoid submitting invalid SSP claims.
Real Time Exemption Checking (RTEC)
- NHSBSA has led the RTEC project since January 2020. CP ITG and Community Pharmacy England have been supportive of its continued roll-out. Read more on RTEC, its phases and continued piloting of Department for Work and Pensions (DWP) RTEC at five pharmacies using PSL at: RTEC. Feedback from RTEC users (PSL/EMIS/Cegedim/Titan/Lloyds/RxWeb systems) has continued to be very positive. Use of RTEC reduces the exchange of paper between pharmacy teams and patients, assisting infection control.
- Contractors are now being encouraged to register for RTEC and more than three quarters of pharmacy organisations have now done so.
- NHSBSA, DWP and the RTEC steering group plan to allow the expansion of the DWP RTEC functionality to additional pharmacy contractors shortly.
- Community Pharmacy England published an RTEC benefits case study (CP ITG Vice Chairman, David Broome).
Apps, wearables and technologies (incl videocon)
NHS App
- NHS App has reached more than 10 million users and become the UK’s most popular app with over 6 million new users since the COVID-19 vaccination status service was added on 17th May 2021. The NHS App is available on the Google Play store and the Apple App store.
- The NHS App team are working on further features including: Personal Health Records (PHRs) integration with NHS App: The first supplier, Patients Know Best, was made available in the NHS App from April 2020 and more are expected to go live in late 2021.
Tool quality and tool frameworks
- NICE is consulting on its plans to amend health technology evaluation. This plan is intended to enable quicker innovation of personalised medicine and digital health technologies.
- Digital Health explored the clinical and regulatory factors of Mobile messaging platforms.
- British Medical Journal (BMJ) analysed over 20,000 mobile health apps on the Google Play Store the majority of which did not properly explain how data was being protected.
- Davey Winder, data security expert explored the design and use of health-related apps.
Apps and tools
- NHS website launched newly designed public-facing profile for pharmacies. The new pharmacy profiles aim to better meet the needs of patients, feature improved support for mobile devices and meet modern accessibility standards.
- ORCHA (the Organisation for the Review of Care and Health Apps) published ‘Digital Health in the UK, National Attitudes and Behaviour Research’, after surveying those who use health apps and those who do not, to provide a snapshot of app use across UK regions and across demographics. Medtech News reported on the related findings.
- Digital Health reported on the launch of NHS Digital Weight Management Programme.
- NHS Test and Trace app expected to be used into 2022, contracts suggest.
- The Government launched COVID Pass Verifier app for businesses to more easily verify the vaccination status or offer proof of a negative test.
- Over three million records were uploaded to the Welsh COVID-19 passport service on launch day.
- A digital physiotherapy tool may save over £1m annually in Wales, pilot results suggest.
- BT reported digital transformation in healthcare, 97% of people who’ve communicated with the health service since the beginning of the pandemic have done so digitally. And 80% of UK health providers believe the need to deliver better remote care is a main driver of digital transformation.
- Combining consumer technology and clinical needs will make health information universally accessible, the vice president of Google Health said.
GP tools
- Babylon announced plans to become a public company following a £2.9bn merger.
- GP at Hand hit a new milestone of 100,000 patients on their GP practice list.
- Over 120 GP practices in London and Manchester have deployed a telephony solution from X-on.
- A GP practice in Milton Keynes has partnered up with Livi to offer video consultations for patients which includes weekend and evening appointments.
Artificial intelligence (AI) and robotics
- HeartFlow tech company explored how gender inequalities might be tackled with help from AI.
- NHS Shared Business Services (SBS) has issued a tender calling for intelligent automation (IA) vendors that supply “off the shelf” automation solutions which would ease NHS administrative task work. The 48-month framework will allow NHS organisations to purchase IA services from pre-approved suppliers, streamlining the process of implementing IA in the health service.
- Pulse reported that NHSX and NHS England are considering the viability of a wider roll out of an AI triage model based on that used by Babylon.
- NHS AI Lab’s “AI in Health and Care Award” backed a further 38 projects with £36 million of funding. These will be backed by NHSX and Accelerated Access Collaborative (AAC).
- The UK’s medicines watchdog has vowed to improve interoperability and collaboration across the health system through smart solutions such as AI.
- AI has been used to predict the structures of almost every protein made by the human body. The development could help the discovery of new medicines.
- The pandemic has shifted views on AI and data use across industries including within the NHS.
- Robotics & Autonomous Systems (UK-RAS) published the report, Preparing the Workforce for 2030: Skills and Education for Robotics & Autonomous Systems.
CPCF/CPCS IT
General
- CPCS IT systems are currently funded centrally by NHSE&I. This arrangement was originally due to end in April 2021 but was extended up until the end of September 2021. CPCS contractors will be responsible for purchasing their own solutions from October 2021 onwards.
- The group has been supportive for guidance and benchmarking that assists the selection of pharmacy contractors’ CPCF/CPCS system supplier and has noted that some contractors will be considering contracts and contract length given that October 1st 2021 is approaching. CP ITG and Community Pharmacy England have supported for continued work but also have fed back to NHSE&I and the CSU at previous and recent meetings that six to twelve months’ notice should be provided ahead of such developments. This time is to allow pharmacy contractors to consider options, agree contracts and train with the new systems. Suppliers also request this period of notice to assist with their allocation of programming resource and to help them with fitting in this work around their other roadmap items.
- Suppliers’ software solutions will need to meet CPCS IT standards set by the NHS. These standards will be reflected in the CPCS Technical Toolkit (which NHSE&I plan to publish in draft format during June 2021 and to iterate it over time as needed). The document incorporates past comments from CP ITG and suppliers.
- Four CPCF IT suppliers are expected to be ready for 1st October 2021: Cegedim, PharmOutcomes, Positive Solutions and Sonar. Other suppliers may come on board later. Suppliers are currently being supported by NHS Digital and NHSBSA to meet the minimum requirements in the CPCS Technical Toolkit. See also: CPCS IT system selection and IT support arrangements.
GP CPCS IT pilot
NHSE&I has been working on the GP CPCS piloting and rollout since 2020 and provided a further update about recent progress:
- The pilot relates to eight London community pharmacies with the Sonar system and four GP practices.
- CPCS connects patients who have a minor illness or need an urgent supply of a medicine with a community pharmacy. CPCS was extended to include referrals from GP practices from 1st November 2020. Pharmacies which are already registered to provide CPCS do not need to re-register to receive referrals from GPs, as this is an extension to the existing Advanced service (previously referrals came only from NHS 111).
- There are a significant number of scenarios in which the GP could refer the patient to the pharmacy.
- NHSE&I have engaged with the LPCs with pilot pharmacies within their areas including with LPCs within Pharmacy London.
GP CPCS IT principles and standards
- When the GP makes a referral to a community pharmacy, this could be done using different types of GP IT (e.g. accuRx or Doctorlink). Contractors have requested common GP CPCS IT standards so that the messages appear seamlessly in pharmacy CPCS IT systems. LPCs have also requested a principle for GPs to have access to a form of IT that enables CPCS referrals to be reported in the appropriate way even for those patients who do not visit the GP practice in person to make it easy for GP practices to divert patients to pharmacy via GP CPSC, where appropriate.
IT policy updates
Integrated Care Systems (ICS) and local digital priorities
- NHSE&I published Designing ICS (June 2019) and Integrating care… (November 2020) setting out plans to increase the importance of ICS within the NHS. Community Pharmacy England published a summary of the key points. ICS were in place by April 2021 (or before in many areas) and ICS have a statutory footing from 2022, subject to legislative change. ICS evolved from Sustainability and Transformation Partnerships. ICSs are to: enable cooperation between the NHS and councils; run services in a coordinated way; agree system-wide priorities; and plan collectively how to improve patients’ day-to-day health. There are around 40 ICS and each of them services populations of between 300,000 and 3 million.
- ICS have been tasked with developing data and digital as one of several key goals (“to drive system working, connect health and care providers, improve outcomes and put the citizen at the heart of their own care”). IT ICS priorities as set out by NHSE&I are as follows: developing Local health and shared care records (LHCRs); preparing digital transformation plans for their area; developing a roadmap for patient-centred digital channels; enabling collaboration including shared appointment booking and referral management and task sharing; publishing statistics; and supporting remote monitoring to allow patients to stay safe at home for longer. Many ICS are forming digital boards and employing digital leads. Local Pharmaceutical Committee Chief Officers have expressed interest with taking on board CP ITG national priorities to support their work with ICS on local digital priorities.
- The group, LPCs and contractors accessing LHCRs are encouraged to attend a Virtual LHCRs/ICS Event: for LPCs and CP ITG (1st July noon-1.30pm).
- Local digital priorities based on feedback received by Community Pharmacy England and on the national CP ITG digital priorities list have been prepared into documents: Local pharmacy digital priorities (prose) and Local pharmacy digital priorities slides. Comments on these documents can be made to it@cpe.org.uk by the end of June 2021.
- Examples of LHCR or local digital priority papers should be sent to it@cpe.org.uk by 30th June 2021.
New CP ITG IT infrastructure survey
- Contractors and others can promote the newly launched survey using template wording. Please can pharmacy contractors and teams also submit an IT arrangements survey response within June. The results will help inform IT policy of system suppliers and the organisations which attend CP ITG.
NHSX and NHS Transformation Unit working to develop a new strategy
- NHSX and NHS Transformation Unit discovery work is continuing to enable the later creation of an NHSX digital strategy for pharmacy, optometry, dentistry, ambulance and community services (PODAC). NHSX are working closely with NHSE&I and other stakeholders to build on the opportunities already taken to accelerate transformation in these areas over the next three to five years.
- Many from within the group volunteered their time to feed into two workshops. Community Pharmacy England and pharmacy teams also fed in via one-to-one interviews with the project team. The project team have explained that some extra system supplier feedback will be captured later. Community Pharmacy England has reported that capturing supplier feedback is also critical.
- Those who have not yet fed in can contact it@cpe.org.uk to be sighted on developments and feedback opportunities.
Pharmacy IT Gantt chart draft template
- System supplier feedback has indicated that multiple projects and objectives are contributing towards severe capacity challenges. Suppliers asked whether the group could explore documenting the multiple projects which are ongoing or forthcoming within the NHS; a draft chart template has been prepared. See: Gantt Chart (slide) and Gantt Chart (spreadsheet). The chart can be set to relate to ‘all contractors’ or can be used as a template by an individual system supplier. Comments about the work may be sent to it@cpe.org.uk.
COVID-19 vaccination programme IT
- More than 600 community pharmacy sites are currently being used to provide vaccines. Contractors have used Point of Care systems such as those provided by Outcomes4Health and Sonar.
- NHSE&I and NHS Digital are supporting the use of the National booking service (NBS) and the wider vaccination programme. NBS enables people to book COVID-19 vaccination appointments at vaccination centres and community pharmacies across England. The national booking service is made up of three parts: (1) an online booking service available to the public on the NHS website – the Book a coronavirus vaccination service; (2) an appointment management system for staff working at vaccination centres and community pharmacies offering vaccinations (Q-Flow); and (3) an app for checking people in to their appointments when they arrive at vaccination centres.
- More than 500 pharmacy-led vaccination sites have administered over five million vaccines across England (as of June 2021). Further pharmacies are being onboarded into the programme.
- Pharmacy teams involved with vaccine supply are encouraged to feed into NHS Digital by registering interest at http://bit.ly/NHS-vaccination-user-research so an NHS Digital team member can get in contact. The user research team are especially interested to hear from those who do activities such as data input or reporting, or those who use computer systems as part of their role.
Other IT policy updates
- The group’s Terms of Reference can be seen here. If you would like to comment on these, please contact it@cpe.org.uk.
- The group’s PMR system wishlist has been further updated during June 2021 and priority and feasibility rankings added. Community pharmacy teams or the group can contact it@cpe.org.uk to take part with further developing iterations to the list.
- CP ITG published a previous progress update, and its quarterly round-up following its last main event.
- Community Pharmacy Digital Group discussed NHS Digital Academy accepting applications during April 2021 (for courses starting from Sept 2021).
Integrated Care Systems and digital technology
- NHSE&I outlined the importance of data and digital in fulfilling plans to progress ICS.
- Derbyshire ICS signed a 10-year shared records deal with Orion Health.
- With ICS set to be put on a statutory footing by 2022, Mala Mawkin says that now is the time to get personal and share stories of integration success.
- Digitalhealth.net published an opinion piece written by a healthcare lawyer putting forward that “putting ICSs on a statutory footing could encourage similar levels of digital maturity across regions if the right funding and governance was in place”, and “success depends on ‘baseline’ digital maturity across organisations”.
- NHSE&I board papers illustrate NHSE&I hopes digital and data will help drive system working as well as connecting health and care providers.
- Infinity Health published an opinion piece about “What the new NHS Integrated Care Systems need to do to be successful” including the expansion of Shared care records, and more proper digital transfers of care.
IT policy updates
- Simon Bolton replaced Sarah Wilkinson as interim chief of NHS Digital.
- The NHSX CEO, explored the digital future of the NHS, including the speculation surrounding NHSX and looked over the work and lessons NHSX has been involved with since it’s set up in 2019.
- NHS Digital improves e-Referral Service (e-RS) further following feedback.
- co.uk reported that NHSE&I is to create a ‘transformation directorate’ merging NHSX with others from NHSE&I. Timothy Ferris was appointed Director Of Transformation for NHSE&I.
- Matt Hancock set out Five mission critical areas of digital health technology.
- DHSC launched a review to highlight how health data can be used for research and analysis.
- Government and healthtech bodies backed a campaign to showcase UK digital health.
- NHSE&I highlighted patient stories of digital primary care in a pandemic.
- Simon Eccles (NHSX CCIO) reflected on the IT leadership survey of 2020 and its findings such as IT Leaders responses demonstrating: more video consultation, a reduction of dissatisfaction with hardware, a shift in attitudes to health data, upgrades being made to records systems and improved online triage becoming more available.
A May 2021 joint Lancet and London School of Economics (LSE) report on the future of the NHS called for a re-evaluation of digital health and for new areas of focus. The suggested focus areas are as follows:
- Deliver integrated electronic health records past commitments (with access for patients, carers, and health and care providers across multiple settings).
- Improve the usability and interoperability of IT systems to reduce staff errors and burnout.
- Address security, privacy and governance concerns.
- Develop easy-to-use platforms for those at risk of digital exclusion.
- Collate datasets to support policy and planning, service delivery, and the precision medicine and public health agendas.
- Invest in IT leadership, training and development of the existing workforce, and the creation of new roles such as data scientists and clinical informaticists
- Understand AI/robotics benefits but as complementary to pre-existing roles and to reduce the burden on staff.
Interoperability and records
Work to update the Pharmacy information flows standard
- The Professional Record Standards Body (PRSB) provided an update at the group’s last meeting and invited CP ITG to a multi-disciplinary workshop, and suppliers to a January 2021 workshop. PRSB pharmacy flows standard developments work was highlighted by Community Pharmacy England. A dedicated pharmacy call with CP ITG and PRSB took place in February 2021. Community Pharmacy England will consider endorsing the dataset after its Service Development Subcommittee have reviewed the latest version of the dataset (which is expected to be available within June 2021). Community Pharmacy England will feed back to PRSB and RPS.
Local health and shared care records (LHCRs) and records update
- Updates about LHCR arrangements have been included within previous progress updates. LHCRs are sometimes referred to as ‘Shared care records / ShCR’.
LPCs and/or local contractors can continue to take steps to gain pharmacy access such as:
- identifying the LHCR project team from the List of records systems;
- learning about case studies such as: Dorset Care Record LHCR pharmacy access case study;
- contacting the LHCR project team and other local partners to find out how to get involved;
- using the ‘Planning pharmacy access briefing’ and frequently updated LHCRs webpage; and
- reviewing the December 2020 Community Pharmacy England/RPS LHCRs/SCR letter to NHS orgs about records access.
Other updates:
- CP ITG pharmacy reps and LPCs will be invited to a Virtual LHCRs Event: Shared care records meeting for LPCs and CP ITG (1st July noon-1.30pm).
- Community Pharmacy England and the Royal Pharmaceutical Society (RPS) called for LHCR standards and continued pharmacy access to Summary Care Records with Additional Information (SCRs with AI) following the COVID-19 pandemic. Read the letter in full here.
- A researcher published their findings on the use of electronic health records (EHRs). They identified benefits but also usability challenges.
- Child health records are set to be digitised earlier than planned (April 2023 instead of a year later) under government plans to give families greater access to their children’s data.
- NHSX plans to launch a new framework for digital social care records.
- Digitalhealth.net published a special report on Local health and shared care records (LHCRs) which argues that the continued growth and development of LHCRs means “the NHS is actually beginning to catch up with what many people think is happening already”.
Other interoperability updates
- DHSC reported that £16 million will be used to introduce digital prescribing across 16 hospitals.
- InterSystems (IT system supplier) expressed the view that interoperability could be key when it comes to unlocking the success of healthcare IT companies.
- Digital health expert Wachter (and author of ‘Using tech to improve the NHS’) believes the world will shortly enter ‘a golden era’ of health IT.
- NHS App e-Referral Service reduces patients who ‘did not attend’ by half.
- Electronic notifications were introduced for pharmacies and GP practices using Sonar and EMIS Web, following the service launch with PharmOutcomes and TPP SystmOne.
- NHS Digital published information on ethnicity recording in the NHS to aid planning and research for COVID-19.
- Amazon progressed further into the US health sector with use of its online pharmacy in the US.
- NHS Wales commits to adoption of GS1 barcode standards.
- PRSB publishes guidance for prescribers using genetic information.
- The group previously agreed to support the capability for anonymised data to be accessible, so that pharmacy teams’ interventions can start to be auditable, and the value of community pharmacy can be better demonstrated. If PMR systems were to be adapted to allow such data sharing, it would require the development of a roadmap and a standard approach to data provision, which may benefit from use of SNOMED CT clinical terms. A PSNC-drafted dataset was prepared and a dataset for the Community Pharmacist Consultation Service could be added. If you would like to help progress this work, please contact it@cpe.org.uk.
NHSmail
- NHSmail support pages outline the benefit with the NHSmail Teams “Virtual Visits” patient consultation platform – it enables appointment booking and video consultation. The NHSmail team provided a demo to Community Pharmacy England and CP ITG representatives. At present, pharmacy team members do not have the ability to ‘switch on’ the functionality and the NHSmail team have advised that an update will be provided later about whether a pharmacy process for accessing this can be added.
- Community Pharmacy England has been working with the NHSmail team to check that pharmacy contractors have the correct revised naming format: ODScode@nhs.net (e.g. not the incorrect format nhspharmacy.ODScode@nhs.net). Contractors who do not have their address within the expected format can raise a ticket with the NHSmail pharmacy admin team.
- Community Pharmacy England has published a factsheet to support escalation of an NHSmail ticket.
- IT case study: Pharmacy and GP practice co-working with NHSmail: Community pharmacy contractors and GP practice staff in Widnes are collaborating more than ever after digitising their communications through a local NHSmail initiative.
IG, identity and security
NHS Digital’s Care Identity Service 2 (CIS2) program
- CIS2 is a future enabler for login to NHS systems without a physical Smartcard for more health and care settings.
- CIS2 (formerly called NHS Identity) is an authentication system. Some newer associated CIS2 integrations are being piloted with health and care professionals in England to prove their identity when accessing national clinical information systems e.g. Summary Care Record (SCR) access on iPads via fingerprint identification by Care Home staff and paramedics.
- Authentication in the future may be via: a specified mobile device correctly set-up and with the right software; or a Smartcard (or virtual equivalent) with or without a direct HSCN connection. However at the present time, Smartcards do require a HSCN connection. There is a piece of work in the pipeline to enable Smartcards to be used on the internet and so remove the reliance on a connection to HSCN.
- At present EPS and the associated authentication being used (CIS1) is limited to Microsoft Windows.
- CIS2 has a series of advantages compared with CIS1: it works with iPads/Windows tablets/laptops, and cross-platform keys, it also works with Google Chrome and Apple Safari instead of just via the Microsoft internet browser.
- Paramedics using CIS2 have found benefits including speedier authentication when compared to older systems.
- Some older CIS1-related technologies will be reaching end-of-life, and NHS Digital and Community Pharmacy England will be communicating about this to suppliers within June 2021.
- Pharmacy contractors, teams and CP ITG have expressed interest in being able to break away from needing to use physical Smartcards, in favour of signing-in on a mobile device and using EPS.
- At some point, CIS2 may be able to create scenarios in which personal mobiles are used for authentication.
- The ongoing work between Entrust and NHS Digital on other ‘Entrust virtual Smartcard certificates’ is separate from CIS2 developments. Work is ongoing to coordinate and align the two projects.
- NHS Digital authentication/CIS2 team have been engaging with each of the pharmacy EPS system suppliers and will continue doing so, and plan to do so further via the EPS Next Generation work and the ongoing NHS Digital / PMR service calls. System suppliers which wish to further understand how to speedily begin the CIS2 integration work should fully explore the NHS Digital CIS2 webpages, continue any PMR/CIS2 team talks which have already begun or contact the CP ITG secretariat (it@cpe.org.uk) who will link you to the CIS2 supplier onboarding team. Suppliers may also contact the CIS2 supplier onboarding team directly.
Data Security and Protection Toolkit (DSPTK)
- Community Pharmacy England has issued communications and guidance relating to the completion of this year’s Toolkit.
- Community Pharmacy England has again worked closely with NHS Digital and contractor testers to keep the workload manageable but the data security protections appropriate. The key differences this year include: new mandatory questions and improvements to the wording for all the questions.
- Community Pharmacy England updated its Data security and information governance hub during April 2021 to support Toolkit completion and published new guidance for the 2020/21 Toolkit submission: Toolkit completion: Five steps to complete the Toolkit (overview); Toolkit completion: Question-by-question guidance (mandatory questions).
- Data security templates were all updated and new ones added: cpe.org.uk/dstemplates. These templates are also now organised both by template number and alphabetically.
- A revised training option was added: Pharmacy data security (for induction or refreshment).
- Community Pharmacy England also hosted meetings with the PMR suppliers and NHS Digital, to help the PMR suppliers with their preparation of PMR-specific guidance for contractors.
- If you would like to feed into the development of the proposed 2021/2022 question set, please email it@cpe.org.uk.
Other updates about data security
- Tributes paid to National Data Guardian Dame Fiona Caldicott who passed away in February 2021. Caldicott passed away at the age of 80 following a career dedicated to seeking the balance between the protection of patient information and the sharing of information to improve care.
- Nicola Byrne has been appointed as the new National Data Guardian (NDG) for Health and Social Care for the next three years. Byrne published an introductory blog and her statement about the reasoning for taking on the role.
- NHS Digital has announced plans to replace the General Practice Extraction Service (GPES) with a new General Practice Data for Planning and Research (GPDPR) service. This new service is intended to make it easier for NHS service planners and researchers to have access to de-personalised data from GPs.
- NHS IT leaders believe Covid has changed attitudes to digital for the positive.
- Community Pharmacy England submitted a consultation response regarding the draft NHSX Records Code. NHSX has closed its consultation and published its Records Management Code of Practice 2020.
- Community Pharmacy England has updated guidance about: Antivirus; Backups; Data handling and Data roles.
- The Irish health service was impacted by a serious cyber-attack during May 2021.
- A cyber security expert summarised some of the increased cyber risks during the pandemic.
Promoting good IT, and user research opportunity
NHS Service Finder enhancements and user research
- NHS Service Finder is a free tool that provides access to information from the Directory of Services (DoS) and the NHS website. It is not accessible by the public, but it does allow pharmacy teams, LPCs and other healthcare professionals to search for service information quickly. The NHS Service Finder team added new enhancements during March 2021 including: restyled search results, quicker searches, and improved filtering options. Community Pharmacy England has been requesting such changes and will continue to provide input to the NHS Service Finder team based on contractor feedback it receives. A YouTube video was published to highlight the benefits for pharmacy team members.
- NHS Digital user researchers are conducting a round of user interviews to help develop the NHS Service Finder tool further. Please take part by emailing it@cpe.org.uk.
Digital tools research by NHS Digital: pharmacy volunteers required
- NHS Digital and NHSX are running research to help identify what community pharmacists and service leads need most from the digital tools and systems that pharmacy teams use on a daily basis at work. They are also looking to identify what information and data pharmacists and service lead staff need in their daily tasks to make informed decisions and best carry out their role. Community Pharmacy England have fed inputs into the project team.
- The user researchers are also looking to speak to pharmacists and service leads, most particularly those working in: regional/local multiples; distance selling pharmacies; and large multiples. They have already spoken with many independent pharmacy contractors. The interviews will take around 45 minutes and can be scheduled at a time that works best for the pharmacy team member.
- NHS Digital user researchers are conducting user interviews to help develop the NHS Service Finder tool further. If you’d like to take part email it@cpe.org.uk with ‘digital tools’ in the subject title.
Other updates: reducing burden
- The group previously identified going paperless as a priority – within its Digital Priority List and Views on the next generation of EPS However, pharmacy teams continue to report considerable use of paper and printing for reasons such as enabling prescription information to move around the dispensary given limited space for PMR terminals. Following work with the group and the paperless sub-group a new ‘Going paperless’ webpage has been published on the Community Pharmacy England website for pharmacy teams.
- Community Pharmacy England published an IT case study in which a Pharmacy in Sheffield went paperless.
- The Government temporarily suspended the requirement for patients (or their representatives) to sign the back of NHS prescription forms or EPS tokens from 1st November 2020 until at least 30th June 2021. Community Pharmacy England continues to discuss with the Department of Health and Social Care (DHSC) the remaining need after this point, for the regulatory requirement that requires the patient or representative to sign a declaration on a prescription form or EPS token when they pay an NHS prescription charge.
- 30,000 iPads will be issued to ambulance crews in England.
- Community Pharmacy England reported on dm+d viewer suppliers welcoming views on new dm+d browsers from pharmacy team and other users: new NHSBSA dm+d browser is in testing mode; NHSBSA’s legacy dm+d browser (available for a limited period); OpenPrescribing dm+d viewer; Unilexon dm+d browser; and East Kent NHS dm+d browser.
- Community Pharmacy England published a new factsheet to explain the EPS tokens ordering and escalation process.
- Case study: How one NHS trust moved to virtual outpatient appointments.
EPS and RTEC
EPS statistics
- NHS Digital EPS and eRD utilisation rate statistics (for the March 2020 dispensing month) are set out on the right, and 95.6% of GP practices were Phase 4 ready at this time. NHSBSA continue to publish EPS dashboards and other data.
- NHSBSA confirmed at the June CP ITG meeting that over 95% of those community pharmacy prescriptions being processed by NHSBSA are now EPS ones. Other statistics at NHSBSA and NHS Digital websites indicate more than 90% of prescriptions are EPS taking into account other dispenser types.
Other EPS and electronic prescribing updates
- NHSBSA’s NHS EPS endorsement guidance has been updated (to version 7.6), pages 13-14. The SSP endorsement can be used from June 2021. The current ‘NCSO workaround’ is being phased out and is scheduled to no longer be allowed to be used from October 2021 dispensing.
- EPS SSPs went live within the June 2021 Drug Tariff with a transition period in which NCSO will be allowed. System suppliers have received guidance from NHSBSA.
- Suppliers may be revising their SSP system-specific guides and Community Pharmacy England offered to comment on drafts.
- NHSBSA and Community Pharmacy England have clarified EPS old patient charge rate processes near the boundary of a new financial year (the patient prescription charge rate typically increases from April 1st each year). If EPS prescriptions are submitted in the March dispensing month, they are processed as ‘old patient charge rate’ and if they are submitted within the April dispensing month they are processed as ‘new patient charge rate’ (i.e. for the new financial year).
- Community Pharmacy England revised its Dose area EPS-related guidance.
- The Welsh government continues to consider an electronic prescription system. Matt Armstrong is feeding into this project on behalf of the CP ITG.
NHS Digital work on EPS Next Generation
- NHS Digital have continued working with NHSX, NHSE&I and others on preparing a newly developed ‘EPS prescribing API / message format’ and EPS Fast Healthcare Interoperability Resources (FHIR) standards. The initial implementation is into secondary care and in relation to homecare providers. The EPS team has rebuilt the existing service using modern standards and technology. It is now available for secondary care and GP suppliers to develop against. It is anticipated that pharmacy system suppliers can start developing from late June 2021 at the earliest.
- The EPS team’s 2021-22 ‘Next generation’ work plan includes progressing a first-of-type within summer 2021 for EPS outpatients and homecare suppliers, and working with suppliers to start the transition and deliver some new EPS features. The 2023-24 the work plan currently includes: identification of further features; building new features; working with suppliers and ideally decommissioning the older HL7 EPS R1 and R2 technology by March 2024.
- NHS Digital have updated several webpages including the following: EPS developer guide, FHIR implementation, FHIR API and signing-in apis.
- One of the main reasons EPS has moved to FHIR is so that there is the ability for EPS suppliers to align with the standard dosage standard – something long campaigned for by the CP ITG’s outgoing Chair.
- The Next Generation EPS features that are being looked at include a range of features, including EPS instalment dispensing for methadone (EPS FP10 MDAs) and EPS antibiotic prescriptions.
- The EPS team would like to be able to work on other EPS wishlist items including: Personally Administered (PADM) items, improvements to cancellation options, removal of the 4-item limit (line item prescribing), extending nomination choices, EPS Tracker APIs, private prescriptions, prescribing and dispensing ‘services’ within directories, customised prison EPS forms, improved eRD (Electronic Repeat Dispensing) and improved dispensing statuses (enabling patient-facing messages via apps etc). Enhancement business cases will be made on a feature-by-feature basis.
- Community Pharmacy England will continue feeding into NHS Digital. The EPS team will also be welcoming more detailed pharmacy team inputs about specific EPS enhancements being worked on such as via upcoming user research events which the group will be made aware of.
- If you work within community pharmacy and would like to feed into the CP ITG’s EPS future list or NHS Digital’s work and events contact it@cpe.org.uk with ‘EPS future’ in the subject title.
Real Time Exemption Checking (RTEC)
- NHSBSA has led the RTEC project since January 2020. CP ITG and Community Pharmacy England have been supportive of its continued roll-out. Read more on RTEC, its phases and continued piloting of Department for Work and Pensions (DWP) RTEC at five pharmacies using PSL at: RTEC. Feedback from RTEC users (PSL/EMIS/Cegedim/Titan systems) has continued to be very positive. Use of RTEC reduces the exchange of paper between pharmacy teams and patients, assisting infection control.
- NHSBSA met with two PMR suppliers across late 2020 to discuss the new data sharing arrangements necessary between NHSBSA and those suppliers. Deployments for pharmacies with those systems had to pause for several months. RTEC deployments relating to those two system suppliers recommenced immediately after the group’s November 2020 meeting, after additional work by NHSBSA and PMR suppliers. Contractors are now being encouraged to register for RTEC and more than three quarters of pharmacy organisations have now done so.
Apps, wearables and technologies (incl videocon)
NHS App
- Details about the NHS App have been explored in past IT progress updates. The NHS App is available on the Google Play store and the Apple App store.
The NHS App team are working on further features including:
- Online consultations integration: The first supplier was made available through the NHS App in 2020 initially with eConsult and Patient Knows Best. The NHS App team is using open standards to help suppliers who provide forms-based triage systems integrate them.
- Push notification capability: The NHS App team have built the ability to allow users to receive broadcast or targeted push notifications and messages relating to their care. This could include reminders for referral appointments, reminders for online consultations, and screening invitations, via services integrated into the app. Suppliers are being onboarded.
- NHS Electronic Referral Service (NHS e-RS) integration: The NHS App team integrated the NHS booking system for hospital appointments, NHS e-RS Manage your referral. This enables patients to book their first hospital appointment when their GP refers them to a specialist.
- Personal Health Records (PHRs) integration with NHS App: The first supplier, Patients Know Best, was made available in the NHS App from April 2020 and more are expected to go live in spring 2021.
Apps and tools
- NHS website launched Flu vaccine finder for patients as reported by Community Pharmacy England.
- An app reviewing firm (for trusts) reported that 80% of apps reviewed do not meet NHS standards.
- Open Access Gov set out the data potential of wearable health technology readings.
- A study recommends that fitness apps should be prescribed to improve physical health, having found that users of wearable fitness trackers walk almost an extra mile a day.
- Push Doctor has relaunched private video consultations via its app after increased demand for it.
- ORCHA reported on a health app download ‘explosion’: a 25% rise in health app downloads since the start of the pandemic – a rise of roughly one million, up from four to five million downloads per day.
- Herefordshire and Worcestershire launches its own health apps library.
- National Institute for Health and Care Excellence (NICE) issued health technologies guidance.
Video consultation, artificial intelligence (AI) and robotics
- GP online reported: Hancock believes GPs should do 45% of consultations remotely post pandemic.
- NHSX has set up an online community to encourage the adoption of robotic process automation (RPA) in health and social care.
- NHSX reported on a year in the life of the NHS AI Lab
- The Scottish government announced an AI strategy for Scotland, including the creation of the Scottish AI Alliance, which will include representation from across society.
Get involved
If you have a related query or would like to feed into the CP ITG or share your updates about IT and digital issues then please don’t hesitate to contact one of the group’s organisers, Dan Ah-Thion or it@cpe.org.uk or you can also sign-up to join the virtual Community Pharmacy Digital Group which helps inform CP ITG’s work with others. You can be involved as much or as little as you like with CPDG, and can unsubscribe from that email group at any time.
Return to the Pharmacy IT hub; CP ITG; CP ITG workstream recent update; or IT a-z index